Choose calcium citrate. It’s absorbed more effectively than calcium carbonate, particularly important for those with lower stomach acid, a common issue with age.
Consider your individual needs. A simple blood test can determine your vitamin D levels; sufficient vitamin D is crucial for calcium absorption. Pair your calcium supplement with a diet rich in vitamin K2, which guides calcium to your bones, rather than soft tissues.
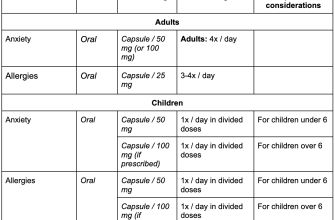
Dosage matters. Aim for the recommended daily intake of calcium, but always consult your doctor or a registered dietitian to personalize your plan. They can help you find the right balance based on your medical history, other medications, and dietary habits. Don’t exceed recommended dosages; high levels of calcium can be harmful.
Remember: This information is for general guidance only and does not replace professional medical advice. Always consult your healthcare provider before starting any new supplement regimen.
- Which Calcium is Best for Osteoporosis?
- Understanding Different Calcium Supplements
- Calcium Citrate vs. Calcium Carbonate: Absorption and Bioavailability
- Stomach Acid and Calcium Absorption
- Dosage Considerations
- Factors Affecting Calcium Absorption: Diet and Medications
- Dietary Factors
- Medication Interactions
- The Role of Vitamin D and Other Nutrients in Calcium Utilization
- Considering Your Individual Needs: Consulting a Doctor
- Beyond Calcium: Lifestyle Choices for Bone Health
- Sunlight and Vitamin D
- Nutrition for Strong Bones
- Other Factors to Consider
- Managing Medications
Which Calcium is Best for Osteoporosis?
Calcium citrate is generally recommended for people with osteoporosis. It’s easily absorbed, regardless of stomach acid levels, making it a suitable choice for older adults who may have reduced stomach acid production.
Calcium carbonate, while less expensive, requires stomach acid for optimal absorption. If you have low stomach acid or take medications that reduce acid production, calcium citrate will likely be more effective.
Consider your individual needs. Speak with your doctor or a registered dietitian to determine the best calcium supplement and dosage for you. They can help you navigate potential drug interactions and tailor a plan to your specific health situation.
Remember to combine calcium supplementation with adequate vitamin D intake. Vitamin D facilitates calcium absorption, enhancing the effectiveness of your supplementation efforts. Your doctor can recommend a suitable vitamin D level and supplementation strategy for your needs.
Dietary changes also play a crucial role. Focus on calcium-rich foods like dairy products, leafy greens, and fortified foods. This contributes to overall bone health and complements your supplementation regimen.
Regular weight-bearing exercise is another vital aspect of osteoporosis management. It strengthens bones and reduces the risk of fractures. Combine this with your nutrition and supplement plan for a holistic approach.
Understanding Different Calcium Supplements
Choosing the right calcium supplement depends on your individual needs and preferences. Let’s explore the common types.
- Calcium Carbonate: This is often the cheapest option and contains a high percentage of calcium. However, it requires stomach acid for absorption, so it’s best taken with food. Consider this if you have good stomach acid production.
- Calcium Citrate: This form is easily absorbed, regardless of stomach acid levels, making it a good choice for people with digestive issues or those taking medications that reduce stomach acid. It is generally more expensive than carbonate.
- Calcium Phosphate: This contains both calcium and phosphorus, which are important for bone health. It’s generally well-tolerated.
- Calcium Magnesium Citrate: Combines calcium and magnesium, another mineral important for bone health and muscle function. May offer benefits beyond calcium alone.
Absorption rates vary slightly between forms. Your doctor can help determine the best option for you based on your medical history and other factors.
- Dosage: Follow recommended daily intake guidelines established by your doctor or health professional.
- Other Nutrients: Consider supplements containing vitamin D, vitamin K2, and magnesium, as they enhance calcium absorption and bone health.
- Food Sources: Remember that a balanced diet rich in calcium-containing foods like dairy, leafy greens, and fortified foods complements supplementation.
Always consult your doctor before starting any new supplement regimen, particularly if you are on other medications or have pre-existing health conditions. They can help assess your individual needs and recommend the appropriate calcium supplement and dosage for optimal bone health.
Calcium Citrate vs. Calcium Carbonate: Absorption and Bioavailability
Calcium citrate boasts superior absorption, particularly for individuals with low stomach acid. This is because citrate dissolves readily in the slightly acidic environment of the stomach, unlike calcium carbonate, which requires a more acidic environment for optimal absorption. Studies show calcium citrate absorption rates reaching up to 40%, compared to calcium carbonate’s variable absorption, often lower, ranging from 15% to 30%, depending on factors such as stomach acid levels and individual digestive health.
Stomach Acid and Calcium Absorption
Individuals with conditions like achlorhydria (low stomach acid production) or those taking antacids that reduce stomach acidity may find calcium citrate much better tolerated and absorbed. This difference in absorption is clinically significant: less calcium carbonate is absorbed, leaving more to be excreted. Calcium citrate offers a more reliable calcium source in these situations. Therefore, for people with lower stomach acid, calcium citrate is generally the preferred choice.
Dosage Considerations
To achieve the same calcium intake, you may need to consume a larger quantity of calcium carbonate due to its lower absorption rate. This can lead to increased risks of side effects like constipation, if higher doses are necessary. Always consult your doctor or a registered dietitian for personalized dosage recommendations, accounting for individual needs and health status.
Factors Affecting Calcium Absorption: Diet and Medications
Maximize calcium absorption by pairing calcium-rich foods with vitamin D. Vitamin D significantly boosts calcium uptake in your gut. Aim for at least 15 mcg (600 IU) of vitamin D daily through sunlight exposure or supplements.
Dietary Factors
Consume calcium with meals. Food, particularly those containing protein and fats, slows digestion and improves calcium absorption. Conversely, high-fiber diets might reduce calcium absorption; balance fiber intake accordingly. Phytates, found in grains and legumes, can also inhibit absorption, thus spacing calcium intake from these foods is beneficial.
Avoid excessive sodium. High sodium intake promotes calcium excretion through urine. Reduce processed foods and salty snacks to improve calcium retention.
Oxalates, in spinach and rhubarb, bind calcium and reduce its absorption. Enjoy these foods moderately and don’t rely solely on them for calcium.
Medication Interactions
Certain medications interfere with calcium absorption. Proton pump inhibitors (PPIs), commonly used for heartburn, reduce stomach acid, hindering calcium uptake. Discuss alternative options with your doctor.
Glucocorticoids, like prednisone, can decrease calcium absorption and increase bone loss. Your physician should closely monitor your calcium levels if you’re taking glucocorticoids.
Some thyroid medications, particularly those containing aluminum, can interfere with calcium. Your doctor can help manage your medication effectively for better calcium absorption.
If you’re taking medications that may impact calcium absorption, consult your doctor or pharmacist to discuss strategies for maximizing calcium benefits and minimizing potential drug interactions.
The Role of Vitamin D and Other Nutrients in Calcium Utilization
Sufficient vitamin D is paramount for calcium absorption. Aim for 600-800 IU daily, increasing as recommended by your doctor, especially if you have limited sun exposure. Regular blood tests monitor your levels.
Magnesium plays a key role in calcium transport into bones. A diet rich in magnesium-containing foods like leafy greens and nuts helps ensure adequate intake. Consult a doctor before starting supplements.
Potassium also supports bone health. Fruits and vegetables are excellent potassium sources, helping maintain calcium balance.
Protein contributes to bone strength. Incorporate lean protein sources like fish, poultry, and beans into your daily diet. Ensure sufficient intake, but avoid excess.
Vitamin K2 directs calcium to bones, reducing the chance of calcium depositing in arteries. Leafy greens are good sources, and supplementation might be considered after consultation with a healthcare professional.
Finally, avoid excessive sodium and caffeine, as they can interfere with calcium absorption. Moderation is key for optimal bone health.
Considering Your Individual Needs: Consulting a Doctor
Schedule a checkup with your doctor or a registered dietitian. They’ll assess your overall health, including bone density, diet, and lifestyle factors influencing bone health. This personalized assessment is crucial.
Discuss your current calcium intake and supplement use. Your doctor can help determine if you’re getting enough calcium from your diet or if supplementation is necessary. They can also help determine the appropriate dosage.
Mention any existing medical conditions or medications you’re taking. Certain health issues and medications can affect calcium absorption or increase the risk of side effects from calcium supplements.
Ask about other bone-building nutrients. Calcium is essential, but Vitamin D, Vitamin K2, and magnesium are also important for bone health. Your doctor can advise on whether you need to supplement these.
Understand potential side effects. Calcium supplements can cause constipation or digestive upset in some individuals. Your doctor will explain the risks and help you choose a safe and well-tolerated supplement.
| Factor | Doctor’s Role |
|---|---|
| Medical History | Identifies potential risks and interactions. |
| Dietary Habits | Evaluates calcium intake from food sources. |
| Bone Density | Assesses the severity of osteoporosis, if present. |
| Lifestyle | Considers exercise, smoking, and alcohol consumption. |
| Supplement Choice | Recommends appropriate type, dosage, and brand. |
Follow your doctor’s recommendations carefully. Regular checkups allow for monitoring your progress and adjustments to your treatment plan as needed.
Beyond Calcium: Lifestyle Choices for Bone Health
Prioritize weight-bearing exercise. Aim for at least 30 minutes most days of the week. Walking, jogging, dancing, and strength training all build bone density. Consider activities that challenge your balance, like Tai Chi or yoga, to reduce fall risk.
Sunlight and Vitamin D
Get adequate sunlight exposure to boost Vitamin D levels. Aim for 10-30 minutes of midday sun on your skin several times a week. Consider a Vitamin D supplement if your levels are low; consult your doctor for testing and dosage recommendations.
Nutrition for Strong Bones
- Include protein in every meal: Aim for lean sources like fish, chicken, beans, and lentils. Protein aids calcium absorption.
- Eat plenty of fruits and vegetables: These provide essential vitamins and minerals for bone health. Focus on leafy greens, broccoli, and berries.
- Choose whole grains over refined grains: They provide more fiber and nutrients.
- Limit processed foods, sugary drinks, and excessive caffeine: These can hinder calcium absorption.
Other Factors to Consider
- Smoking Cessation: Smoking significantly increases bone loss. Quitting dramatically improves bone health.
- Alcohol Moderation: Excessive alcohol consumption interferes with calcium absorption and increases fracture risk. Limit your intake.
- Regular Check-ups: Schedule regular bone density screenings with your doctor, especially if you have a family history of osteoporosis.
Managing Medications
Certain medications, such as corticosteroids, can negatively impact bone health. Discuss any concerns about medications and their effect on bone health with your doctor. They can help you manage potential side effects and develop strategies to mitigate bone loss.