Directly switching from metoprolol to bisoprolol often involves a 1:1 dose conversion for similar efficacy. However, individual patient responses vary, so close monitoring of blood pressure and heart rate is critical after the change.
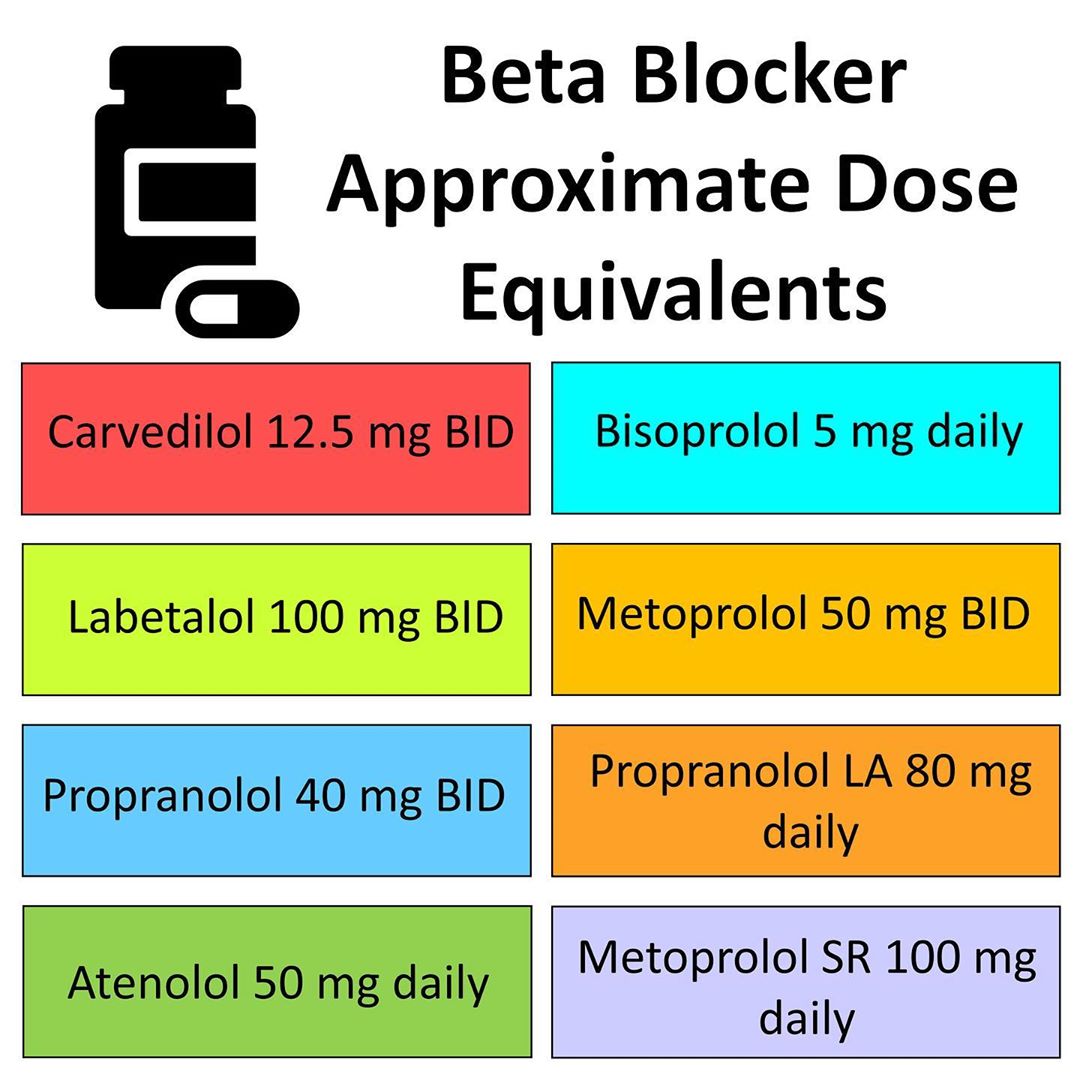
Consider starting with the equivalent dose of bisoprolol and carefully titrating upward or downward as needed, based on the patient’s clinical response. This approach allows for personalized medication adjustments. Remember to account for the different formulations (immediate-release vs. extended-release) when making the conversion. For example, if a patient takes metoprolol succinate (extended-release), the equivalent bisoprolol dosage should be based on the sustained-release formulation.
Regular monitoring, including blood pressure checks and assessment of symptoms like dizziness or bradycardia, are paramount following the conversion. Adjusting the dose may be required depending on these observations. This personalized approach ensures patient safety and optimizes treatment effectiveness. Always consult with a healthcare professional before initiating any dosage changes.
Key takeaway: While a 1:1 dose conversion serves as a reasonable starting point, individual adjustments are often necessary for optimal results. Patient-specific monitoring is the cornerstone of a successful metoprolol to bisoprolol transition.
- Metoprolol to Bisoprolol Conversion: A Practical Guide
- Monitoring the Transition
- Adjusting the Dosage
- Calculating the Equivalent Dose
- Factors Affecting Dose Conversion
- Example Conversion
- Monitoring for Adverse Effects During Conversion
- Frequency of Monitoring
- Specific Adverse Effects and Management
- Patient Education
- Follow-up
- Considerations for Specific Patient Populations
Metoprolol to Bisoprolol Conversion: A Practical Guide
Begin by carefully reviewing the patient’s medical history and current metoprolol dosage. Titration is key; abrupt cessation of metoprolol can be harmful. Generally, a 1:1 conversion ratio of metoprolol tartrate to bisoprolol is recommended. For example, a patient taking 100mg of metoprolol tartrate daily can transition to 100mg of bisoprolol daily. However, this is a starting point – individual responses vary significantly. Close monitoring is vital.
Monitoring the Transition
Regular blood pressure and heart rate checks are crucial during the conversion period. Expect potential side effects like dizziness, fatigue, or nausea, particularly in the initial days. These usually subside. Adjust the bisoprolol dose incrementally based on the patient’s response, guided by clinical judgment and monitored parameters. Patients should be educated to report any significant symptoms promptly to their healthcare provider.
Adjusting the Dosage
If side effects are pronounced, consider reducing the bisoprolol dose temporarily, then gradually increase it again to the target dose over several weeks. If blood pressure or heart rate remains unsatisfactory, a different beta-blocker or alternative treatment may be necessary. Always prioritize patient safety and well-being. Regular follow-up appointments allow for accurate assessment and personalized adjustments to the treatment plan.
Calculating the Equivalent Dose
Generally, a 1:1 ratio of metoprolol succinate to bisoprolol is used for conversion. This means that 100mg of metoprolol succinate is considered equivalent to 10mg of bisoprolol. However, this is a simplification. Individual patient responses vary.
Factors Affecting Dose Conversion
Heart rate and blood pressure should be closely monitored during conversion. Adjust the bisoprolol dose based on the patient’s response. Start with a lower dose of bisoprolol and titrate upwards slowly, carefully observing the patient’s reaction.
Renal function influences drug metabolism. Patients with impaired kidney function may require dose adjustments. Consult relevant guidelines for dosage modification in renal impairment.
Always refer to current clinical guidelines and your institution’s protocols for optimal dose adjustments. A phased approach, starting low and gradually increasing, is advised to minimise side effects.
Example Conversion
A patient currently takes 200mg of metoprolol succinate daily. A suitable starting dose of bisoprolol would be 20mg daily (200mg metoprolol / 10mg bisoprolol per 100mg metoprolol = 20mg bisoprolol). However, remember to monitor closely and adjust based on the patient’s clinical status.
Disclaimer: This information is for educational purposes only and does not constitute medical advice. Always consult with a healthcare professional before making any changes to your medication.
Monitoring for Adverse Effects During Conversion
Closely monitor patients for bradycardia, hypotension, and worsening heart failure symptoms. Check blood pressure and heart rate frequently, especially during the initial titration phase.
Frequency of Monitoring
- Monitor vital signs (heart rate, blood pressure) daily for the first week of conversion.
- Then, monitor vital signs at least weekly for the following four weeks.
- Adjust monitoring frequency based on individual patient response and stability.
Pay close attention to any reported dizziness, lightheadedness, or fatigue. These symptoms may indicate a need for dose adjustment or a slower titration schedule.
Specific Adverse Effects and Management
- Bradycardia: If heart rate drops below 50 bpm or symptoms develop, consider reducing the bisoprolol dose or temporarily withholding it. Consult with a cardiologist.
- Hypotension: If systolic blood pressure falls significantly, adjust the bisoprolol dose downward or use a slower titration schedule. Monitor fluid status.
- Worsening Heart Failure: Closely observe for signs of worsening heart failure, such as increased shortness of breath, edema, or weight gain. If symptoms worsen, reduce the bisoprolol dose or consider alternative medications.
- Bronchospasm: Bisoprolol may worsen bronchospasm in susceptible individuals. Monitor respiratory function closely, particularly in patients with a history of asthma or COPD. Consider alternative beta-blockers if bronchospasm occurs.
- Peripheral Vascular Disease: Observe for worsening symptoms of peripheral vascular disease, such as coldness or numbness in extremities. Dose reduction may be necessary.
Patient Education
Educate patients about potential side effects and the importance of reporting any new or worsening symptoms. Encourage them to keep a record of their vital signs and symptoms.
Follow-up
Schedule regular follow-up appointments to assess the patient’s response to the conversion and adjust therapy as needed. This allows for timely detection and management of adverse effects.
Considerations for Specific Patient Populations
Patients with Chronic Obstructive Pulmonary Disease (COPD): Proceed cautiously. Bisoprolol’s bronchoconstricting effects might exacerbate COPD symptoms. Closely monitor respiratory function during conversion.
Patients with Heart Failure: Bisoprolol is generally preferred in heart failure due to its favorable effects on mortality. However, careful titration is necessary, particularly in those with severe heart failure. Monitor for worsening symptoms.
Patients with Renal Impairment: Reduce the bisoprolol dose based on creatinine clearance. Consult renal dosing guidelines for precise adjustments.
Patients with Hepatic Impairment: Lower doses of both metoprolol and bisoprolol might be necessary. Closely monitor for drug accumulation.
Elderly Patients: Start with a lower dose of bisoprolol and titrate slowly, observing for adverse effects such as bradycardia or hypotension. Regular monitoring is key.
Diabetic Patients: Bisoprolol can mask symptoms of hypoglycemia. Closely monitor blood glucose levels, especially initially.
Patients with Peripheral Artery Disease (PAD): Bisoprolol may worsen symptoms in PAD patients due to its potential to reduce blood flow to the extremities. Exercise caution and monitor for worsening symptoms.
Patients on other medications: Check for potential drug interactions before and during conversion. Consult a drug interaction database if needed. This includes interactions with calcium channel blockers, digoxin, insulin, and other beta blockers.