No, azithromycin and penicillin are entirely different antibiotics. Azithromycin belongs to the macrolide class, while penicillin is a beta-lactam antibiotic. They target bacteria through different mechanisms. This key difference means that someone allergic to penicillin can often tolerate azithromycin.
This distinction is critical for patient safety. A penicillin allergy can trigger serious reactions, ranging from mild skin rashes to life-threatening anaphylaxis. Doctors carefully consider a patient’s allergy history before prescribing antibiotics. If you have a penicillin allergy, always inform your doctor or pharmacist; they will choose an appropriate alternative, like azithromycin in many cases.
However, no antibiotic is universally safe. While azithromycin is usually well-tolerated, potential side effects include nausea, vomiting, and diarrhea. Rarely, more serious reactions may occur. Always discuss any concerns about medication with your healthcare provider before taking azithromycin or any other drug. They can assess your individual health situation and prescribe the safest and most effective treatment.
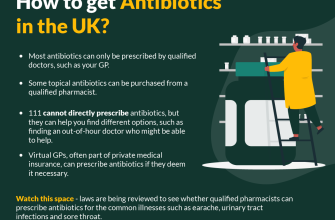
Remember, self-medicating with antibiotics is dangerous. Improper antibiotic use can lead to antibiotic resistance, making infections harder to treat. Always consult a medical professional for diagnosis and treatment of bacterial infections.
- Does Azithromycin Have Penicillin in It?
- Understanding the Differences
- Why This Distinction Matters
- Important Note: Consult Your Doctor
- Azithromycin’s Class: A Macrolide, Not a Penicillin
- Understanding Macrolides
- Key Differences & Implications
- When to Consult a Doctor
- Penicillin’s Mechanism of Action: Beta-lactam Ring
- Azithromycin’s Mechanism of Action: Binding to Ribosomes
- Cross-reactivity and Allergic Reactions: Understanding the Differences
- Allergic Reactions to Azithromycin
- Penicillin Allergy and Azithromycin Prescription
- Common Misconceptions About Azithromycin and Penicillin
- Seeking Medical Advice: When to Consult a Doctor
- When to Consider a Doctor’s Visit for Azithromycin Use
- Understanding Your Medication
Does Azithromycin Have Penicillin in It?
No, azithromycin does not contain penicillin. They belong to completely different classes of antibiotics.
Understanding the Differences
Azithromycin is a macrolide antibiotic, while penicillin is a beta-lactam antibiotic. These are distinct chemical structures with different mechanisms of action against bacteria.
- Azithromycin works by binding to bacterial ribosomes, preventing protein synthesis and bacterial growth.
- Penicillin inhibits bacterial cell wall synthesis, leading to bacterial death.
Why This Distinction Matters
This difference is critical for individuals with penicillin allergies. Penicillin allergies are common and can range from mild skin reactions to life-threatening anaphylaxis. Since azithromycin is not a penicillin, individuals allergic to penicillin can usually tolerate azithromycin without issue. However, always inform your doctor about any allergies before taking any medication.
Important Note: Consult Your Doctor
While azithromycin and penicillin are different, other antibiotics might share similar structures or mechanisms. Always consult your doctor or pharmacist before starting any new medication, even if you believe it’s safe. They can assess your medical history, current health conditions, and potential drug interactions to ensure the medication is appropriate for you.
- Discuss your medical history, including allergies.
- Explain your symptoms and the prescribed treatment.
- Ask any questions regarding potential side effects or interactions.
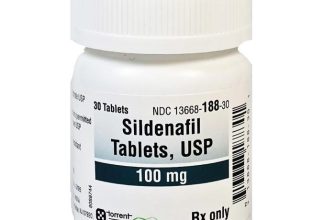
Azithromycin’s Class: A Macrolide, Not a Penicillin
No, azithromycin does not contain penicillin. It belongs to a completely different class of antibiotics: the macrolides.
Understanding Macrolides
Macrolides, like azithromycin, work by binding to bacterial ribosomes, preventing protein synthesis and thus killing bacteria. This mechanism differs significantly from that of penicillins, which inhibit bacterial cell wall synthesis.
Key Differences & Implications
This distinction is crucial for patients with penicillin allergies. Because azithromycin is a macrolide, individuals allergic to penicillin can usually tolerate azithromycin without experiencing a reaction. However, it’s always vital to inform your doctor about any allergies before taking any medication. Allergic reactions, though rare, can still occur with azithromycin.
When to Consult a Doctor
Always consult your physician or pharmacist before using azithromycin or any medication. They can assess your individual needs, determine appropriate dosage, and manage potential interactions with other medications you might be taking.
Penicillin’s Mechanism of Action: Beta-lactam Ring
Penicillin’s power lies in its unique beta-lactam ring. This four-membered cyclic amide structure is the key to its antibiotic properties. The ring’s strained structure makes it highly reactive.
Specifically, penicillin targets bacterial enzymes called penicillin-binding proteins (PBPs). These PBPs are crucial for building bacterial cell walls. Penicillin irreversibly binds to the active site of these enzymes.
This binding inhibits the synthesis of peptidoglycan, a major component of bacterial cell walls. Without a functioning cell wall, bacteria become vulnerable and eventually die due to osmotic lysis. Different penicillins vary slightly in their structure, leading to variations in their PBP affinity and bacterial spectrum.
Understanding the beta-lactam ring is vital for comprehending penicillin’s mode of action and the development of antibiotic resistance. Resistance often arises from bacterial mutations affecting the PBPs’ active sites, hindering penicillin binding.
Azithromycin’s Mechanism of Action: Binding to Ribosomes
Azithromycin fights bacterial infections by directly targeting their protein synthesis machinery. It achieves this by binding to the bacterial ribosome’s 50S subunit.
Specifically, azithromycin interacts with the 23S ribosomal RNA (rRNA) within the 50S subunit. This binding interferes with peptidyl transferase activity.
- Peptidyl transferase is the enzyme responsible for forming peptide bonds between amino acids during protein synthesis.
- Azithromycin’s binding inhibits this crucial step, halting bacterial protein production.
This inhibition leads to a disruption in bacterial growth and ultimately, bacterial death. The drug’s specific binding site ensures selectivity, minimizing effects on human ribosomes (which differ structurally).
- The high concentration of azithromycin achieved within phagocytic cells enhances its activity against intracellular bacteria.
- This prolonged intracellular persistence contributes to its efficacy against a wide range of infections.
Remember, though azithromycin targets bacterial ribosomes, its mechanism differs from that of penicillin, which inhibits bacterial cell wall synthesis.
Cross-reactivity and Allergic Reactions: Understanding the Differences
Azithromycin and penicillin belong to different antibiotic classes; therefore, cross-reactivity is unlikely. However, allergic reactions are distinct from cross-reactivity. Cross-reactivity implies an allergic response to one drug triggering a reaction to a structurally similar drug. Allergic reactions, on the other hand, result from your immune system incorrectly identifying a substance (like azithromycin) as harmful.
Allergic Reactions to Azithromycin
Symptoms range from mild skin rashes and itching to severe reactions such as anaphylaxis (a life-threatening condition involving breathing difficulties and circulatory collapse). If you experience any allergic symptoms after taking azithromycin, seek immediate medical attention. Previous penicillin allergies don’t automatically predict an azithromycin allergy, but they do warrant caution. Always inform your doctor of any past drug allergies.
Penicillin Allergy and Azithromycin Prescription
Doctors carefully consider patient histories. While a penicillin allergy doesn’t guarantee an azithromycin allergy, it prompts careful monitoring for any potential reactions. Your doctor may opt for alternative antibiotics if your history suggests a higher risk of reaction. Open communication with your healthcare provider is key to safe medication use.
Common Misconceptions About Azithromycin and Penicillin
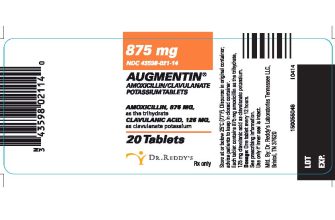
Azithromycin and penicillin are completely different antibiotics. They belong to distinct classes – azithromycin is a macrolide, while penicillin is a beta-lactam. This key difference impacts how they work in the body and which infections they treat.
Myth 1: They’re interchangeable. This is false. Doctors prescribe specific antibiotics based on the type of infection. Switching between them without a doctor’s guidance is dangerous and can lead to treatment failure or antibiotic resistance.
Myth 2: Azithromycin is a “stronger” penicillin. Azithromycin isn’t a penicillin at all. Its mechanism of action differs significantly, impacting bacterial susceptibility. One is not inherently “stronger” than the other; effectiveness depends on the specific bacteria causing the infection.
Myth 3: Allergic reactions are identical. While both can trigger allergic reactions, the symptoms and severity can vary. A penicillin allergy doesn’t automatically mean an azithromycin allergy, and vice versa. Always inform your doctor about any medication allergies.
Myth 4: They treat the same infections. The spectrum of bacteria they target varies. Penicillin is often effective against strep throat, while azithromycin might be preferred for some types of pneumonia. Your doctor will determine the appropriate antibiotic based on your diagnosis.
Always consult your doctor or pharmacist for accurate information and guidance regarding your medication. Never self-medicate or change prescriptions without professional advice.
Seeking Medical Advice: When to Consult a Doctor
If you have an allergy to any medication, especially penicillin, always consult your doctor before taking azithromycin or any other antibiotic. This is crucial for your safety.
Seek immediate medical attention if you experience a severe allergic reaction, such as difficulty breathing, swelling of your face or throat, or hives. These symptoms require prompt medical intervention.
Contact your physician if you experience persistent symptoms, such as a high fever lasting longer than three days, or worsening symptoms despite taking azithromycin. Don’t wait for symptoms to resolve themselves.
When to Consider a Doctor’s Visit for Azithromycin Use
Consider scheduling an appointment with your doctor before starting azithromycin if you have pre-existing medical conditions, such as liver or kidney problems, heart rhythm issues, or a history of prolonged QT interval. These conditions can interact negatively with azithromycin.
Additionally, discuss potential interactions with other medications you are currently taking. Azithromycin can interact with various drugs. Your doctor will provide guidance on any necessary precautions.
Understanding Your Medication
| Symptom | Action |
|---|---|
| Mild side effects (e.g., nausea, diarrhea) | Monitor symptoms. Contact your doctor if they persist or worsen. |
| Severe allergic reaction | Seek immediate medical help. This is a medical emergency. |
| Unusually high fever or worsening symptoms | Contact your doctor. A different treatment may be necessary. |
| Pre-existing medical conditions | Consult your doctor before starting treatment. |
Regular communication with your healthcare provider ensures safe and effective medication use. Always inform your doctor about all medications, supplements, and allergies you have.