Prescribe amoxicillin-clavulanate for bacterial infections resistant to amoxicillin alone. This combination combats bacteria producing beta-lactamases, enzymes that inactivate amoxicillin. Understanding the precise mechanism of action is key to successful treatment.
Amoxicillin targets bacterial cell wall synthesis, halting bacterial growth and ultimately causing cell death. Clavulanate, the beta-lactamase inhibitor, prevents the breakdown of amoxicillin by these enzymes. This synergistic effect broadens the antibiotic’s spectrum significantly, making it effective against a wider range of infections. Remember to always consider patient-specific factors, such as allergies and renal function, before prescribing.
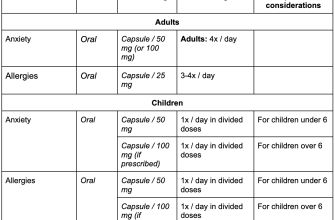
Common infections successfully treated include respiratory tract infections (like pneumonia and bronchitis), skin and soft tissue infections, and urinary tract infections. However, consider resistance patterns in your region when choosing this antibiotic. Always perform culture and sensitivity testing whenever feasible to ensure appropriate treatment and avoid unnecessary antibiotic use. Consult the latest guidelines for specific dosage recommendations based on age and infection severity. Proper adherence to treatment duration is critical to prevent relapse.
Note: This information serves as a concise overview. Always refer to comprehensive prescribing information for detailed instructions and potential side effects. Monitor patients closely for any adverse reactions. Responsible antibiotic use is crucial for minimizing the development of antibiotic-resistant bacteria.
- Amoxicillin Beta-Lactamase Inhibitors: A Detailed Overview
- Understanding Beta-Lactamase Enzymes
- The Role of Amoxicillin in Bacterial Infections
- Common Beta-Lactamase Inhibitors Combined with Amoxicillin
- Mechanism of Action: How Inhibitors Work with Amoxicillin
- Spectrum of Activity: Which Bacteria are Affected?
- Clinical Uses and Indications for Amoxicillin/Inhibitor Combinations
- Potential Side Effects and Drug Interactions
- Considerations for Prescribing and Patient Counseling
Amoxicillin Beta-Lactamase Inhibitors: A Detailed Overview
Amoxicillin, a widely used antibiotic, sometimes faces challenges due to bacterial beta-lactamases, enzymes that break down the antibiotic, rendering it ineffective. To combat this, amoxicillin is often combined with a beta-lactamase inhibitor.
Clavulanate potassium is the most common partner. This combination, amoxicillin/clavulanate (brand names include Augmentin), effectively inhibits beta-lactamases, allowing amoxicillin to reach its target and kill bacteria. The ratio of amoxicillin to clavulanate varies depending on the specific formulation.
Sulbactam is another beta-lactamase inhibitor frequently paired with ampicillin, not amoxicillin. This combination is effective against certain bacteria producing beta-lactamases, offering a therapeutic alternative in specific situations. Note that this combination does not include amoxicillin.
Choosing the right combination depends on the bacterial infection. Doctors consider factors like the type of bacteria, severity of the infection, patient’s allergies, and potential side effects. Always consult a healthcare professional for diagnosis and treatment.
Common side effects of amoxicillin/clavulanate include diarrhea, nausea, and vomiting. Serious allergic reactions, though rare, can occur. Patients should report any unusual symptoms immediately to their doctor. Specific prescribing information should be obtained from the product labeling.
The development of bacterial resistance remains a significant concern. Responsible antibiotic use, including completing prescribed courses of medication, is vital in slowing the emergence of resistant strains. Overuse or misuse of antibiotics should be avoided.
Research continues to explore new beta-lactamase inhibitors and improve existing combinations, aiming to enhance treatment effectiveness and address the challenge of antibiotic resistance. This ongoing research ensures continuous improvements in treating bacterial infections.
Understanding Beta-Lactamase Enzymes
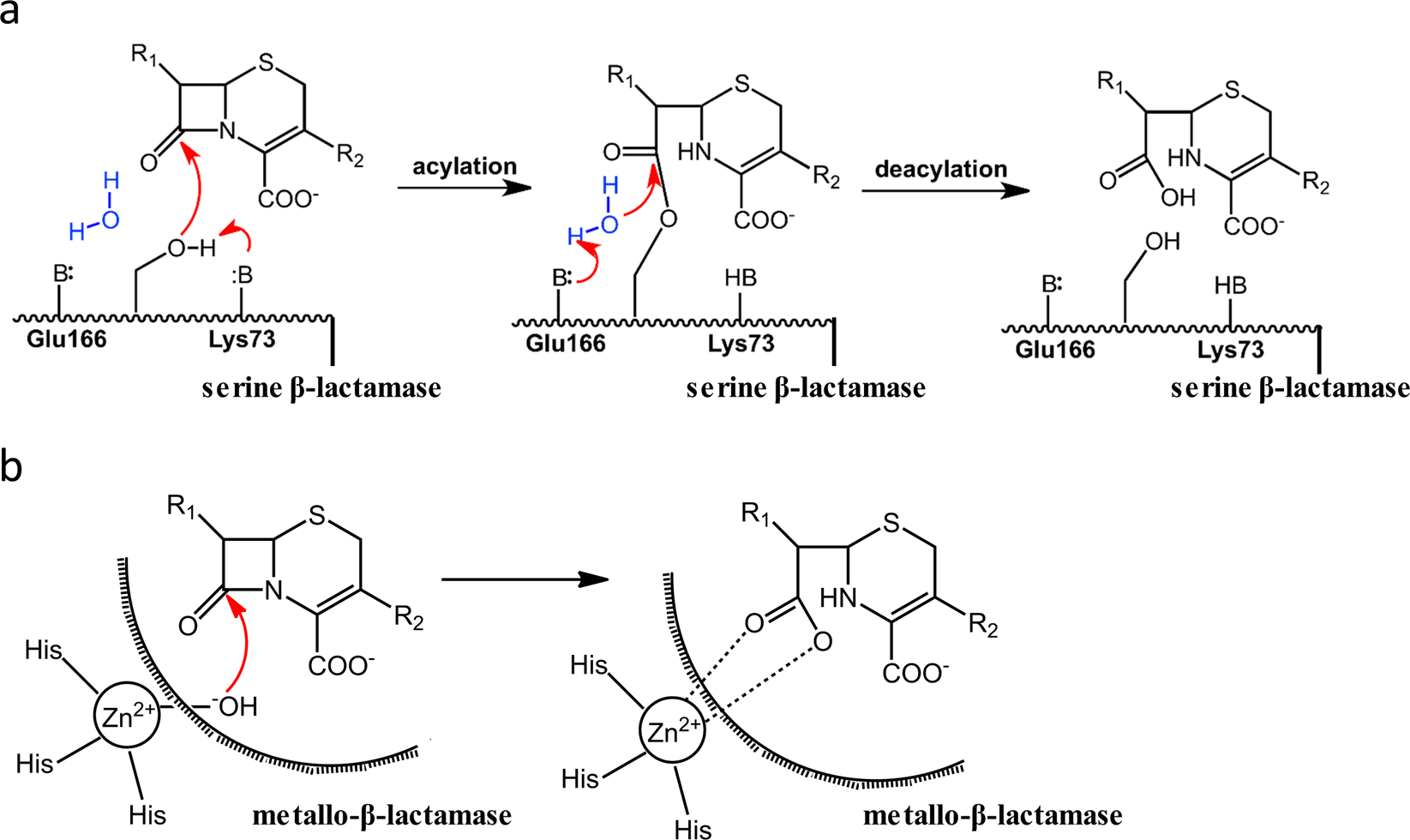
Beta-lactamases are enzymes produced by bacteria to resist the effects of beta-lactam antibiotics, like amoxicillin. They function by hydrolyzing the beta-lactam ring, the crucial part of the antibiotic molecule responsible for its antibacterial action. This process renders the antibiotic ineffective.
Several factors influence beta-lactamase activity:
- Enzyme Class: Different classes (A, B, C, D) exhibit varying substrate specificities and sensitivities to inhibitors.
- Bacterial Species: The type and amount of beta-lactamase varies considerably between bacterial species.
- Environmental Conditions: pH and temperature affect enzyme activity.
Understanding the mechanisms of beta-lactamases is vital for developing effective antibiotic strategies. This includes:
- Beta-Lactamase Inhibitors: These molecules, like clavulanate or sulbactam, bind to and inactivate beta-lactamases, protecting the antibiotic from hydrolysis.
- Antibiotic Design: Designing antibiotics that resist beta-lactam hydrolysis is a key focus of research.
- Combination Therapy: Using antibiotics with different mechanisms of action alongside beta-lactam antibiotics can circumvent resistance.
Specific examples of beta-lactamases include TEM, SHV, and CTX-M enzymes. These enzymes are frequently associated with resistance to extended-spectrum cephalosporins and other beta-lactam antibiotics. Knowing the specific beta-lactamase produced by a bacterium guides appropriate antibiotic selection.
Monitoring the prevalence of beta-lactamases and their specific types is crucial for effective infection control and treatment strategies. Regular surveillance and antibiotic stewardship programs aid in this process.
The Role of Amoxicillin in Bacterial Infections
Amoxicillin effectively targets a wide range of common bacterial infections. It’s a first-line treatment for many conditions, including strep throat, ear infections, and some respiratory infections. Its success hinges on its ability to disrupt bacterial cell wall synthesis, ultimately leading to bacterial death.
However, its effectiveness varies depending on the bacteria involved. Amoxicillin primarily combats gram-positive bacteria and some gram-negative bacteria. Against certain strains, resistance has emerged, necessitating the use of beta-lactamase inhibitors. These inhibitors prevent the breakdown of amoxicillin by bacterial enzymes.
Dosage depends on several factors, including the patient’s age, weight, and the severity of the infection. Always follow your doctor’s instructions. Incorrect dosage can lead to treatment failure or the development of resistant strains.
| Bacterial Infection | Amoxicillin Efficacy | Considerations |
|---|---|---|
| Strep Throat | High | Usually a short course of treatment |
| Ear Infections (Otitis Media) | High (in many cases) | May require combination with other antibiotics for certain infections |
| Pneumonia | Variable | Effectiveness depends on the causative bacteria; often used in combination with other antibiotics |
| Skin Infections | Variable | Dependent on the infecting bacteria; often requires stronger antibiotics |
Potential side effects include diarrhea, nausea, and allergic reactions, though these are relatively uncommon. Always inform your doctor of any allergies or pre-existing medical conditions before starting amoxicillin. Early diagnosis and treatment are key to successful outcomes.
Common Beta-Lactamase Inhibitors Combined with Amoxicillin
Amoxicillin’s effectiveness against bacteria producing beta-lactamases is significantly enhanced when combined with a beta-lactamase inhibitor. Two common pairings are amoxicillin/clavulanate and amoxicillin/sulbactam.
Amoxicillin/clavulanate is widely available and used to treat a broad spectrum of bacterial infections, including respiratory tract infections, skin and soft tissue infections, and urinary tract infections caused by beta-lactamase-producing bacteria. Clavulanate potassium effectively inhibits many beta-lactamases, protecting amoxicillin from degradation.
Amoxicillin/sulbactam offers a similar spectrum of activity, particularly effective against certain gram-negative bacteria. Sulbactam, another beta-lactamase inhibitor, provides broad-spectrum coverage, often employed when resistance to clavulanate is suspected or observed. This combination is frequently used for treating intra-abdominal and gynecological infections.
The choice between amoxicillin/clavulanate and amoxicillin/sulbactam often depends on the suspected pathogen and local resistance patterns. Your doctor will consider these factors when prescribing the appropriate combination for your specific infection.
Remember to always follow your doctor’s instructions regarding dosage and duration of treatment. Complete the full course of antibiotics, even if symptoms improve, to prevent recurrence of infection and the development of antibiotic resistance.
Mechanism of Action: How Inhibitors Work with Amoxicillin
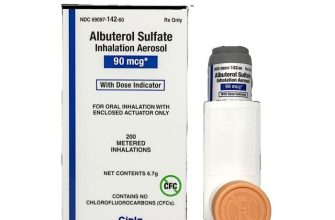
Amoxicillin, a penicillin antibiotic, fights bacterial infections by inhibiting bacterial cell wall synthesis. However, some bacteria produce beta-lactamases, enzymes that break down amoxicillin, rendering it ineffective. Beta-lactamase inhibitors counteract this.
These inhibitors, such as clavulanate or sulbactam, bind to and inactivate beta-lactamases. This protection allows amoxicillin to reach its target and effectively inhibit bacterial cell wall synthesis. The combination significantly broadens the spectrum of activity against beta-lactamase-producing bacteria.
The mechanism is synergistic: the inhibitor protects amoxicillin, enhancing its antibacterial power. This isn’t a simple additive effect; the combined action is substantially greater than the sum of individual actions.
| Inhibitor | Mechanism of Action | Effect on Amoxicillin |
|---|---|---|
| Clavulanate | Irreversibly binds to beta-lactamases | Protects amoxicillin from degradation |
| Sulbactam | Inactivates beta-lactamases through acylation | Enhances amoxicillin’s efficacy against resistant strains |
Consequently, amoxicillin combined with a beta-lactamase inhibitor treats infections caused by bacteria resistant to amoxicillin alone. This combination therapy offers a valuable treatment option for various bacterial infections.
Spectrum of Activity: Which Bacteria are Affected?
Amoxicillin combined with a beta-lactamase inhibitor, like clavulanate or sulbactam, significantly broadens its antibacterial activity.
This combination targets a wider range of bacteria compared to amoxicillin alone, effectively combating those that produce beta-lactamases – enzymes that break down amoxicillin, rendering it ineffective.
- Gram-positive bacteria: Streptococcus pneumoniae (many strains, but resistance is emerging), Staphylococcus aureus (methicillin-sensitive strains), Streptococcus pyogenes.
- Gram-negative bacteria: Haemophilus influenzae, Moraxella catarrhalis, Escherichia coli (some strains), Klebsiella pneumoniae (some strains), Proteus mirabilis.
- Anaerobes: Bacteroides fragilis (some strains), other anaerobic bacteria commonly found in infections.
However, remember that resistance is a growing concern. The spectrum of activity can vary depending on the specific beta-lactamase inhibitor used and the bacterial strain.
- Always check local antibiograms to understand prevalent bacterial resistance patterns in your region.
- Culture and sensitivity testing should guide antibiotic selection for optimal treatment.
- Appropriate antibiotic use helps prevent the development of further resistance.
Therefore, relying solely on this information for treatment decisions is inadequate. Consult up-to-date clinical guidelines and consider local resistance patterns for informed prescribing.
Clinical Uses and Indications for Amoxicillin/Inhibitor Combinations
Amoxicillin combined with a beta-lactamase inhibitor, such as clavulanate or sulbactam, treats a wide range of bacterial infections. These combinations effectively overcome bacterial resistance caused by beta-lactamases, enzymes that break down amoxicillin.
Common uses include treating infections of the respiratory tract, such as sinusitis, bronchitis, and pneumonia. They’re also effective against skin and soft tissue infections, including cellulitis and abscesses. Furthermore, these combinations are frequently prescribed for urinary tract infections and ear infections (otitis media).
Specific indications often depend on the infecting organism and local antibiotic resistance patterns. Always consult local guidelines and susceptibility testing to ensure optimal treatment. For example, while generally effective against Streptococcus pneumoniae, resistance variations exist, necessitating appropriate testing.
Amoxicillin/clavulanate is often preferred for community-acquired pneumonia, while amoxicillin/sulbactam might be considered for certain intra-abdominal infections. Dosage and treatment duration vary based on the infection’s severity, patient factors, and the specific antibiotic used.
Remember that these combinations are not effective against all bacteria. They are inappropriate for treating infections caused by organisms inherently resistant to beta-lactam antibiotics, such as Pseudomonas aeruginosa or Enterococcus faecalis. Appropriate antibiotic selection requires careful consideration of the suspected pathogen.
Potential Side Effects and Drug Interactions
Amoxicillin-clavulanate combinations, while generally well-tolerated, can cause side effects. These usually are mild and transient, but you should contact your doctor if they become bothersome or severe.
- Gastrointestinal Issues: Diarrhea is the most common side effect. Nausea, vomiting, and abdominal pain may also occur. Staying hydrated and consuming bland foods can help alleviate these issues. Severe diarrhea requires immediate medical attention.
- Skin Reactions: Rashes, hives, and itching are possible. In rare instances, more severe allergic reactions, including angioedema (swelling of the face, lips, tongue, or throat) and anaphylaxis, can occur. Seek immediate medical help for any serious allergic reaction.
- Other potential side effects: Headache, dizziness, and changes in taste can also happen. These usually subside as treatment progresses.
Drug interactions can affect the effectiveness of amoxicillin-clavulanate or increase the risk of side effects. Therefore, it’s critical to inform your doctor about all medications, supplements, and herbal remedies you’re currently taking. Here are some key drug interactions to be aware of:
- Oral contraceptives: Amoxicillin-clavulanate may reduce the effectiveness of some oral contraceptives. Discuss alternative birth control methods with your doctor during treatment.
- Methotrexate: Concurrent use can increase the risk of methotrexate toxicity. Close monitoring is necessary.
- Warfarin: This combination may increase the risk of bleeding. Regular blood tests are crucial to monitor the effects.
- Probenecid: Probenecid can increase the blood levels of amoxicillin, potentially leading to higher risks of side effects.
This information is not exhaustive. Always consult your doctor or pharmacist for a complete list of potential side effects and drug interactions specific to your situation and health status. They can provide personalized advice based on your individual needs and medical history.
Considerations for Prescribing and Patient Counseling
Always confirm the patient’s allergies before prescribing any beta-lactam antibiotic. A thorough allergy history, including reactions to penicillin, is critical.
Assess the patient’s renal function, especially in older adults or those with pre-existing kidney disease. Dosage adjustments may be necessary based on creatinine clearance.
Instruct patients to complete the full course of amoxicillin-clavulanate, even if symptoms improve early. Stopping treatment prematurely can lead to treatment failure and potential antibiotic resistance.
Advise patients about potential side effects, such as diarrhea, nausea, vomiting, and rash. Explain the importance of contacting their doctor if these side effects become severe or persistent.
Counsel patients on appropriate food and drink consumption. Amoxicillin-clavulanate can be taken with or without food, but maintaining consistent intake is recommended.
Warn patients about potential interactions with other medications, especially anticoagulants and oral contraceptives. Discuss appropriate alternative contraception if necessary.
Monitor patients closely for signs of Clostridium difficile-associated diarrhea, including persistent diarrhea and abdominal cramping. This is a rare but serious side effect.
For patients with mild to moderate infections, consider alternative antibiotics if possible to minimize antibiotic resistance.
Ensure patients understand the importance of proper hygiene practices, particularly handwashing, to prevent the spread of infection.
Provide clear, concise instructions for taking the medication, including dosage, frequency, and duration. Use patient-friendly language and avoid medical jargon.