Experiencing prolonged cycles while on Clomid? Don’t panic. Many women encounter longer cycles than expected during Clomid treatment. Understanding the reasons behind this is key to managing the situation effectively. Factors such as your age, ovarian reserve, and response to the medication all contribute to cycle length.
A longer Clomid cycle doesn’t automatically signify failure. Your doctor will carefully monitor follicle development using ultrasound scans and blood tests to assess your response. This monitoring allows for adjustments in dosage or treatment strategies if necessary. Open communication with your doctor is vital throughout the process, ensuring you receive personalized guidance.
Consider tracking your basal body temperature (BBT) and cervical mucus changes. This information, coupled with your doctor’s guidance, can help you pinpoint ovulation and better understand your cycle patterns. Remember, patience and consistent communication are crucial for navigating this aspect of fertility treatment. Your doctor can discuss alternative treatment plans if Clomid proves ineffective after a few cycles of extended length.
Key takeaway: Prolonged cycles on Clomid are common. Regular monitoring, open communication with your physician, and proactive cycle tracking empower you to manage this aspect of treatment effectively. Don’t hesitate to raise your concerns with your doctor during each appointment.
- Clomid Long Cycles: A Detailed Guide
- Understanding Clomid and Long Cycles
- Strategies for Managing Long Clomid Cycles
- When to Seek Further Assistance
- Understanding Clomid Long Cycles: Protocol and Mechanism
- Benefits and Potential Risks of Clomid Long Cycles
- Monitoring and Management During Clomid Long Cycles
- Blood Test Schedule
- Ultrasound Monitoring
- Managing Side Effects
- Understanding Cycle Length Variation
- Alternative Treatments
- Clomid Long Cycles vs. Alternative Treatments
- Letrozole
- Gonadotropins
- Intrauterine Insemination (IUI)
- In Vitro Fertilization (IVF)
- Treatment Comparison
- Surgical Options
Clomid Long Cycles: A Detailed Guide
If you’re experiencing prolonged cycles while using Clomid, understand that this isn’t uncommon. Several factors contribute to this, including your individual response to the medication, underlying hormonal imbalances, and even the specific Clomid dosage. Let’s explore these potential causes and discuss management strategies.
Understanding Clomid and Long Cycles
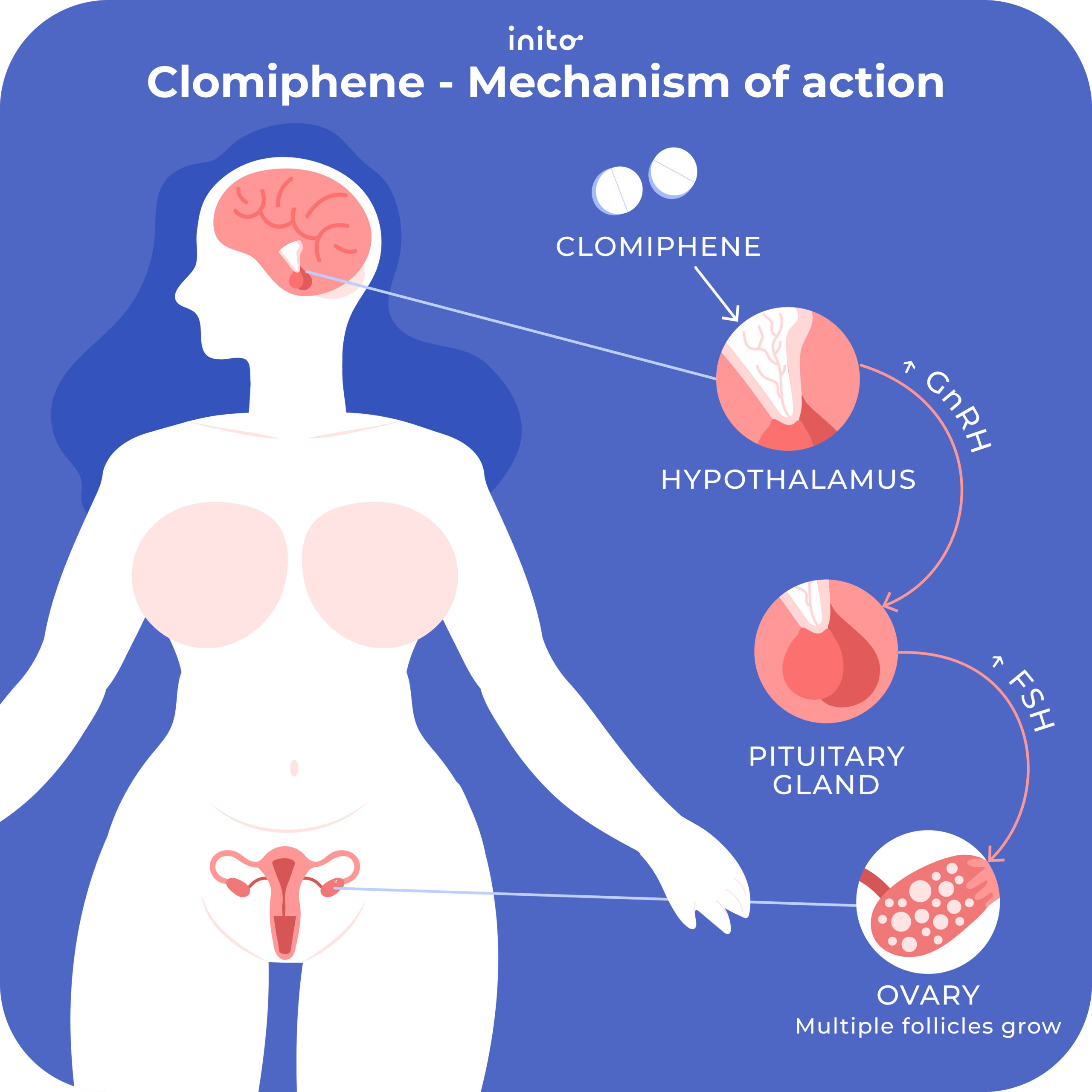
Clomid (clomiphene citrate) stimulates ovulation by impacting your hypothalamus and pituitary gland, ultimately increasing the production of follicle-stimulating hormone (FSH) and luteinizing hormone (LH). However, the response varies significantly between individuals. Some women experience shorter cycles, while others experience prolonged cycles–cycles exceeding 35 days. This can result from insufficient follicle growth, delayed or absent ovulation, or other hormonal irregularities. A thorough blood test monitoring FSH, LH, estradiol, and progesterone levels will pinpoint the problem.
Dosage plays a significant role. Higher dosages aren’t always better; they can sometimes hinder proper follicular development and lead to delayed or absent ovulation, resulting in longer cycles. Similarly, pre-existing conditions such as polycystic ovary syndrome (PCOS) or thyroid problems can impact Clomid’s effectiveness and cycle length.
Strategies for Managing Long Clomid Cycles
Your fertility specialist will likely adjust your Clomid dosage based on your response and blood test results. They may increase or decrease the dosage depending on the observed follicular development and hormonal patterns. In some cases, they might add other medications, such as metformin (for PCOS) or other ovulation-inducing drugs if Clomid alone is insufficient. Regular monitoring through ultrasound scans is critical to assess follicular development and predict ovulation.
Lifestyle modifications also matter. Maintaining a healthy weight, eating a balanced diet, and exercising regularly can significantly impact hormone production and improve your chances of a successful outcome. Stress reduction techniques, like yoga or meditation, can also be beneficial, as stress can interfere with hormonal balance and ovulation. Open communication with your physician is paramount; proactive discussion about your concerns will lead to better management and treatment.
When to Seek Further Assistance
Persistent long cycles despite adjustments in dosage and lifestyle changes warrant a thorough review of your treatment plan. Your doctor may suggest alternative fertility treatments, such as intrauterine insemination (IUI) or in vitro fertilization (IVF), if Clomid proves ineffective. Remember, seeking professional guidance is crucial for achieving optimal results and ensuring your well-being.
Understanding Clomid Long Cycles: Protocol and Mechanism
Clomid long cycles typically involve taking Clomiphene citrate (Clomid) daily for a longer period, often 5-10 days, rather than the standard 5 days. This extended administration aims to stimulate the ovaries more consistently, potentially improving follicular growth and increasing the chances of ovulation and pregnancy.
The mechanism differs slightly from standard Clomid protocols. Prolonged exposure to Clomid influences the hypothalamic-pituitary-ovarian axis differently. The extended stimulation can lead to a more sustained increase in follicle-stimulating hormone (FSH) and luteinizing hormone (LH), resulting in a greater number of follicles developing. However, this increased stimulation also carries a higher risk of ovarian hyperstimulation syndrome (OHSS).
A typical protocol involves initiating Clomid around days 3-5 of the menstrual cycle and continuing daily for 5-10 days. Close monitoring through blood tests (measuring estrogen and hormone levels) and ultrasound scans (assessing follicular development) is crucial for proper management. The doctor will adjust the dosage and duration based on your response to treatment.
Dosage adjustments depend on individual responses and potential side effects. Blood tests monitor hormone levels, preventing overstimulation. Ultrasound scans visualize follicle development, guiding decisions on triggering ovulation with hCG (human chorionic gonadotropin) if needed. This personalized approach minimizes risks and optimizes the chances of a successful outcome.
Remember, Clomid long cycles are not suitable for everyone. Your fertility specialist should carefully assess your medical history and current health before recommending this protocol. Open communication with your doctor is vital throughout the treatment process.
Benefits and Potential Risks of Clomid Long Cycles
Doctors sometimes prescribe longer Clomid cycles to improve ovulation chances. This extended use may increase the likelihood of multiple follicles developing, leading to a higher chance of pregnancy with twins or triplets. However, it’s vital to understand that this increased chance also raises the risk of pregnancy complications.
Increased risk of ovarian hyperstimulation syndrome (OHSS) is a significant concern with prolonged Clomid use. OHSS can cause severe abdominal pain, bloating, and even require hospitalization. The severity depends on individual factors and response to the medication.
While longer cycles might boost pregnancy odds, they don’t guarantee success. The chance of pregnancy remains variable and depends on various factors, including female age and overall reproductive health. Furthermore, extended Clomid use doesn’t reduce the risk of miscarriage.
Another potential downside is a higher likelihood of developing medication-resistant cycles. This means future attempts may require alternative treatments or higher dosages of Clomid, increasing the risk of associated side effects. Discuss all potential risks and benefits thoroughly with your physician before starting longer Clomid cycles.
Close monitoring of ovarian response through regular ultrasound scans and blood tests is necessary during extended cycles. This allows for timely adjustments in medication and minimizing risks. Your doctor will tailor the treatment plan to your individual circumstances and needs.
Remember, this information is for educational purposes only and doesn’t substitute professional medical advice. Always consult with your doctor to determine the best course of action for your unique situation.
Monitoring and Management During Clomid Long Cycles
Regular monitoring is key. Expect frequent appointments, typically including blood tests to track hormone levels (estradiol, progesterone, LH) and ultrasound scans to monitor follicle growth and endometrial thickness. These tests help your doctor precisely time ovulation and assess the cycle’s progress.
Blood Test Schedule
- Estradiol levels: Monitored to assess follicle development, typically every 2-3 days after starting Clomid.
- Progesterone levels: Checked after ovulation to confirm successful egg release and luteal phase development.
- LH surge: Detected to pinpoint the precise timing of ovulation.
Ultrasound Monitoring
- Initial baseline ultrasound: Establishes a starting point for follicle assessment.
- Follow-up ultrasounds: Provide ongoing evaluation of follicle growth and endometrial lining. Frequency varies depending on individual response.
- Ovulation confirmation ultrasound: Verifies follicle rupture and confirms ovulation.
Your doctor will adjust your medication or treatment plan based on these results. This might involve modifying Clomid dosage, adding other medications (like gonadotropins for poor response), or adjusting the timing of intercourse or intrauterine insemination (IUI).
Managing Side Effects
Common side effects include hot flashes, headaches, mood swings, and ovarian cysts. Open communication with your doctor is vital. They can offer strategies to manage these symptoms, such as pain relievers for headaches or lifestyle adjustments for hot flashes. Report any significant discomfort immediately.
Understanding Cycle Length Variation
Clomid long cycles are variable. Your cycle might be significantly longer than a typical 28-day cycle. Don’t be alarmed by this variation, as long as it’s being carefully monitored by your doctor. Follow their guidance regarding medication, testing, and timing of intercourse or IUI.
Alternative Treatments
If Clomid long cycles are consistently unsuccessful, your doctor may discuss other fertility treatments, such as different ovulation induction medications or assisted reproductive technologies (ART), like IVF.
Clomid Long Cycles vs. Alternative Treatments
If Clomid long cycles aren’t yielding results, consider these alternatives. Your doctor will help determine the best option for you based on your individual circumstances and medical history.
Letrozole
Letrozole is an aromatase inhibitor that can stimulate ovulation. Studies show it’s often as effective as Clomid, potentially with fewer side effects for some women. Discuss potential benefits and risks with your doctor.
Gonadotropins
These fertility medications, such as follicle-stimulating hormone (FSH) and luteinizing hormone (LH), directly stimulate the ovaries. They’re a more potent option than Clomid or Letrozole, used when other treatments fail to induce ovulation. Expect closer monitoring with this approach.
Intrauterine Insemination (IUI)
IUI involves placing sperm directly into the uterus, increasing the chances of fertilization. It’s often used in conjunction with ovulation stimulation medications like Clomid, Letrozole, or gonadotropins. Success rates vary based on individual factors.
In Vitro Fertilization (IVF)
IVF is a more involved procedure where eggs are retrieved from the ovaries, fertilized in a lab, and then implanted back into the uterus. It’s a more aggressive approach, reserved for cases where other treatments haven’t been successful. This method offers higher chances of pregnancy, but it’s resource-intensive and more expensive.
Treatment Comparison
| Treatment | Mechanism | Success Rate | Side Effects |
|---|---|---|---|
| Clomid | Stimulates ovulation | Varies; lower than other options | Hot flashes, ovarian cysts |
| Letrozole | Inhibits estrogen production | Comparable to Clomid; potentially fewer side effects | Headaches, joint pain |
| Gonadotropins | Direct ovarian stimulation | Higher than Clomid or Letrozole | Ovarian hyperstimulation syndrome (OHSS) risk |
| IUI | Direct sperm placement | Moderate; depends on other factors | Mild discomfort |
| IVF | In vitro fertilization and embryo transfer | Higher than other options | Multiple; requires consultation |
Remember, this information isn’t a substitute for medical advice. Consult your doctor to discuss your options and choose the best treatment plan for you.
Surgical Options
In some cases, underlying conditions like blocked fallopian tubes or endometriosis might require surgical intervention before pursuing fertility treatments. Your doctor will assess your situation and determine if surgery is necessary.