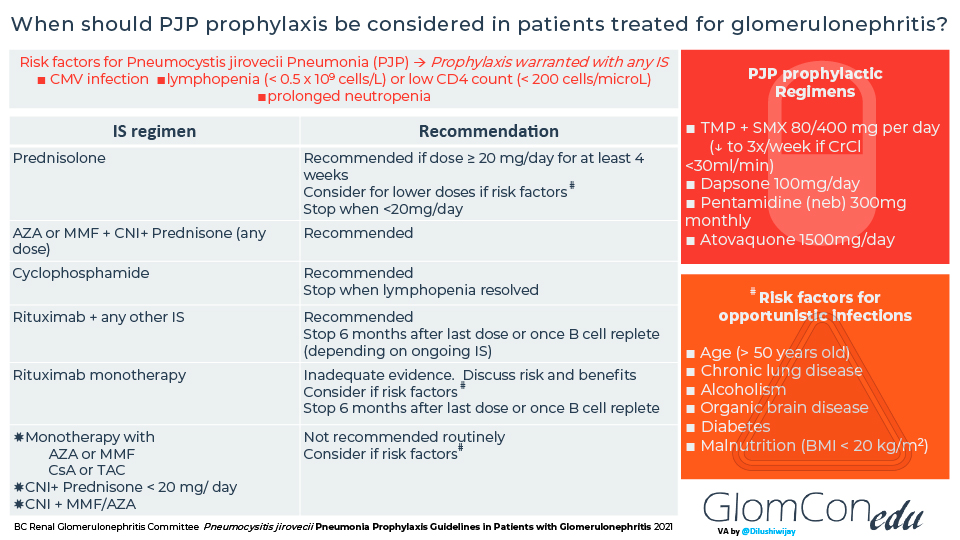
Prescribe Bactrim prophylaxis cautiously, reserving it for individuals with specific risk factors for opportunistic infections like Pneumocystis jirovecii pneumonia (PCP) – namely, those with CD4 counts below 200 cells/mm³ or a history of PCP. This targeted approach minimizes unnecessary antibiotic use and reduces the risk of antibiotic resistance.
For patients meeting these criteria, a typical regimen involves sulfamethoxazole-trimethoprim (Bactrim) DS (double-strength) once daily. Adjust dosage based on individual kidney function, always consulting relevant guidelines and lab results for personalized medication management. Regular monitoring of complete blood counts and liver function tests is recommended to detect potential adverse effects.
Remember, prophylactic Bactrim isn’t a universal solution. Consider alternative medications or strategies for individuals with documented allergies or intolerance to sulfamethoxazole. Furthermore, consistent adherence to the prescribed regimen is paramount for optimal prevention. Discuss potential drug interactions with other medications the patient may be taking.
Note: This information serves as a brief summary and should not replace consultation with updated clinical guidelines and expert medical advice. Always prioritize individualized patient care based on their specific circumstances and medical history. Always refer to official guidelines for the most current recommendations.
- Bactrim Prophylaxis Guidelines
- Specific Patient Populations
- Dosage and Duration
- Monitoring and Side Effects
- Alternative Prophylaxis Options
- Contraindications
- Conclusion
- Indications for Bactrim Prophylaxis: Identifying High-Risk Patients
- Dosage and Administration: Optimizing Prophylactic Efficacy
- Specific Considerations
- Monitoring for Adverse Effects and Drug Interactions: Ensuring Patient Safety
- Specific Monitoring Considerations
- Patient Education and Communication
- Alternatives to Bactrim Prophylaxis: Considering Other Options
- Alternative Antibiotics for Specific Situations
- Non-Antibiotic Approaches
- Individualized Prophylaxis Strategies
Bactrim Prophylaxis Guidelines
Prescribe Bactrim prophylaxis cautiously, considering potential risks and benefits for each patient.
Specific Patient Populations
- Pneumocystis jirovecii pneumonia (PCP) prophylaxis in HIV-positive individuals: Target CD4 counts below 200 cells/mm³. Consider alternative prophylaxis if Bactrim allergy exists. Monitor for side effects, including rash and blood disorders. Regular CD4 monitoring is vital.
- Toxoplasmosis prophylaxis in HIV-positive individuals: Indicated for those with a history of toxoplasmosis infection and CD4 counts below 100 cells/mm³. Again, consider alternatives if Bactrim allergy is present. Careful monitoring for adverse reactions is needed.
- Prophylaxis for recurrent urinary tract infections (UTIs): Reserve for patients with frequent, documented UTIs resistant to other antibiotics. Consider culture and sensitivity testing before prescribing. Evaluate for potential underlying anatomical issues.
Dosage and Duration
Dosage depends on the indication and patient factors. Always refer to the most up-to-date prescribing information. Duration of prophylaxis varies: PCP prophylaxis is generally lifelong once initiated at a low CD4 count; UTI prophylaxis duration should be carefully evaluated with the patient.
Monitoring and Side Effects
- Regularly monitor complete blood counts (CBC) to detect potential hematological side effects.
- Assess for hypersensitivity reactions, including skin rashes and allergic reactions.
- Instruct patients to report any unusual symptoms promptly to their healthcare provider.
- Assess renal function, especially in patients with pre-existing kidney disease.
Alternative Prophylaxis Options
Alternatives to Bactrim include Dapsone, atovaquone/proguanil, and pentamidine. Selection depends on patient-specific factors, including allergies and comorbidities. A physician should always weigh the risks and benefits when choosing an appropriate regimen.
Contraindications
- Known allergy to sulfonamides or trimethoprim.
- Severe hepatic or renal impairment.
- Pregnancy, especially during the first trimester and close to delivery.
- Breastfeeding (carefully weigh risks and benefits).
Conclusion
Bactrim prophylaxis should be individualized, guided by specific patient needs and careful monitoring. Always consult updated guidelines and consider alternative options when necessary.
Indications for Bactrim Prophylaxis: Identifying High-Risk Patients
Bactrim prophylaxis is recommended for individuals with recurrent urinary tract infections (UTIs), specifically those experiencing three or more UTIs within a year. This preventative measure significantly reduces the likelihood of future infections.
Patients with a history of complicated UTIs, such as those involving kidney infection (pyelonephritis) or requiring hospitalization, also benefit from Bactrim prophylaxis. These infections often indicate underlying structural abnormalities or functional issues requiring ongoing protection.
Individuals with anatomical abnormalities predisposing them to UTIs, like vesicoureteral reflux (VUR) or neurogenic bladder, should be considered for Bactrim prophylaxis to mitigate the high risk of recurrent infection. Regular prophylaxis helps maintain urinary tract health.
Immunocompromised patients, including those with HIV or undergoing chemotherapy, are at heightened risk for serious bacterial infections. Bactrim prophylaxis offers a crucial layer of protection against opportunistic infections, such as those caused by Pneumocystis jirovecii.
Before initiating Bactrim prophylaxis, a thorough assessment of the patient’s medical history, including allergies and potential drug interactions, is necessary. This proactive approach ensures patient safety and optimizes treatment efficacy.
Regular monitoring for potential adverse effects, such as allergic reactions or the development of antibiotic-resistant bacteria, is important during Bactrim prophylaxis. This close observation allows for timely intervention and adjustments to the treatment plan.
Dosage and Administration: Optimizing Prophylactic Efficacy
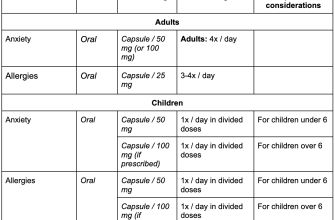
For adults, the typical Bactrim prophylactic dosage is one double-strength tablet (containing 800 mg sulfamethoxazole and 160 mg trimethoprim) daily. Children’s dosages vary significantly based on weight and should always follow the physician’s prescription. Precise adherence to the prescribed schedule is paramount for maintaining consistent drug levels and preventing resistance. Skipped doses weaken protection.
Specific Considerations
Patients with renal impairment require dosage adjustments. Lower doses are necessary to prevent accumulation and toxicity. Your doctor will calculate the appropriate dose based on your creatinine clearance. Similarly, hepatic impairment may influence drug metabolism, necessitating individualized dose modifications. Always inform your physician about any existing kidney or liver conditions.
Prophylactic Bactrim should be taken with a full glass of water to minimize gastrointestinal upset. Taking it with food might slightly reduce nausea, but this should be discussed with your prescribing physician. Regular blood tests may be recommended to monitor for adverse effects, such as hematologic changes. Promptly report any unusual bleeding, bruising, or fatigue.
Monitoring for Adverse Effects and Drug Interactions: Ensuring Patient Safety
Regularly monitor patients for common Bactrim side effects, including nausea, vomiting, diarrhea, and rash. These usually resolve with continued treatment, but report any severe or persistent symptoms immediately. Blood tests, particularly complete blood counts (CBCs), should be considered before initiating Bactrim prophylaxis, especially in patients with known hematologic abnormalities or a history of bone marrow suppression. These should also be repeated periodically, depending on the patient’s risk factors and duration of therapy. Frequency depends on factors such as patient risk and treatment duration – consult the latest guidelines.
Specific Monitoring Considerations
Pay close attention to signs of hypersensitivity reactions, such as skin reactions (Stevens-Johnson syndrome, toxic epidermal necrolysis). These are rare but serious. Discontinue Bactrim immediately if such reactions occur and provide appropriate supportive care. Kidney function should be assessed before starting and periodically during long-term therapy through serum creatinine monitoring, especially in patients with pre-existing renal impairment. Liver function tests (LFTs) may be warranted in patients with liver disease or risk factors for liver toxicity. Monitor for signs of drug interactions, particularly with warfarin (increased bleeding risk), methotrexate (increased methotrexate toxicity), and certain diuretics (potential for electrolyte imbalances).
Patient Education and Communication
Educate patients about potential side effects and the importance of reporting any concerning symptoms. Provide clear instructions on medication adherence and the need for follow-up appointments for monitoring. Emphasize the importance of informing healthcare providers of all other medications, herbal supplements, and allergies to ensure safe and effective use of Bactrim. This proactive approach helps minimize risks and maximize patient safety.
Alternatives to Bactrim Prophylaxis: Considering Other Options
If Bactrim isn’t suitable, several alternatives exist. Nitrofurantoin offers a viable option for urinary tract infection (UTI) prophylaxis, particularly in women. Its efficacy is well-documented, and it presents a different resistance profile compared to Bactrim.
Alternative Antibiotics for Specific Situations
For individuals with sulfa allergies, consider antibiotics like trimethoprim alone (if the infection is caused by susceptible organisms), or fluoroquinolones like ciprofloxacin. However, fluoroquinolone use should be judicious due to growing resistance patterns. Always confirm susceptibility testing before prescribing.
Non-Antibiotic Approaches
Cranberry supplements can help prevent UTIs in some individuals by inhibiting bacterial adhesion to the urinary tract. While not a replacement for antibiotics in all cases, it might be considered as an adjunct therapy or for individuals with recurrent UTIs seeking to reduce antibiotic use. Remember: Consult with a physician before starting cranberry supplementation, especially if on other medications.
Individualized Prophylaxis Strategies
The best alternative depends heavily on individual factors like allergy history, infection history, and presence of comorbidities. A thorough evaluation including culture and sensitivity testing is critical to guide treatment choices and optimize patient outcomes. Close monitoring is necessary regardless of the prophylactic agent used.