Avoid taking ibuprofen or naproxen with warfarin. These nonsteroidal anti-inflammatory drugs (NSAIDs) increase the risk of bleeding, significantly impacting warfarin’s anticoagulant effect. Always discuss alternative pain relievers with your doctor before taking any medication while on warfarin.
Similarly, avoid St. John’s Wort. This herbal supplement interacts negatively with warfarin, potentially reducing its effectiveness and raising the chance of dangerous blood clots. This interaction is well-documented and requires careful attention. Choose safer alternatives for mood support, and consult your physician or pharmacist.
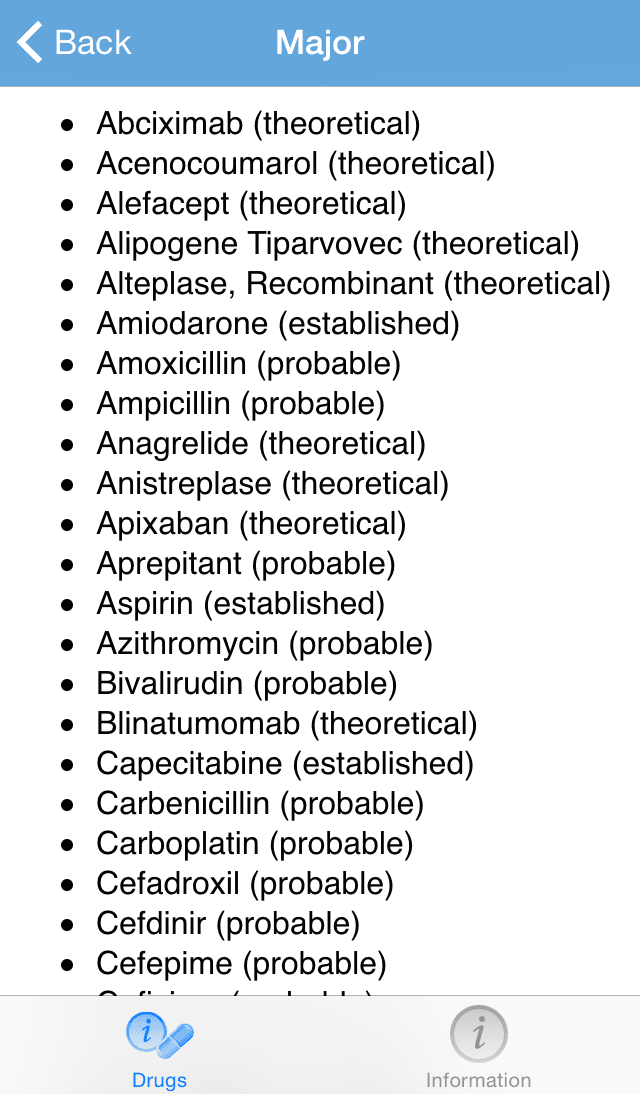
Many antibiotics also pose a risk. Specific medications, like certain types of fluoroquinolones and sulfonamides, can amplify warfarin’s effects, leading to excessive bleeding. Always inform your doctor and pharmacist of all antibiotics you are taking or plan to take. They can suggest safe alternatives or adjust your warfarin dose accordingly. This proactive approach protects your health.
Note: This information is not exhaustive. Always consult your doctor or pharmacist before starting or stopping any medication while taking warfarin. They possess the specialized knowledge to guide you safely through your treatment.
Remember: This list highlights common medications. Numerous other drugs can interact with warfarin. Open communication with your healthcare team is your best defense against dangerous drug interactions.
- Medications Contraindicated with Warfarin
- Understanding Warfarin’s Mechanism of Action
- Impact on Clotting Factors
- Consequences of Reduced Clotting
- Factors Influencing Warfarin’s Effect
- Monitoring Warfarin Therapy
- In Summary
- Nonsteroidal Anti-Inflammatory Drugs (NSAIDs) and Warfarin Interactions
- Increased Bleeding Risk
- Alternatives to NSAIDs
- Aspirin and Warfarin: A Risky Combination
- Antibiotics and the Risk of Increased Bleeding
- Antibiotics to Watch Out For
- Herbal Supplements and Warfarin: Potential for Dangerous Interactions
- The Impact of Amiodarone on Warfarin’s Efficacy
- Monitoring Your Medications While on Warfarin
- The Importance of Open Communication with Your Doctor
- Consequences of Ignoring Contraindications: Bleeding Risks and Management
- Recognizing Warning Signs
- Managing Bleeding Complications
- Preventing Future Complications
Medications Contraindicated with Warfarin
Warfarin, a blood thinner, interacts negatively with many medications. Careful monitoring is crucial for patients on warfarin. Avoid concurrent use without your doctor’s explicit approval.
Certain antibiotics, such as ciprofloxacin and metronidazole, can increase warfarin’s effects, raising your bleeding risk. Similarly, some antifungals, like ketoconazole, share this risk.
Nonsteroidal anti-inflammatory drugs (NSAIDs), including ibuprofen and naproxen, can also increase bleeding risk when combined with warfarin. Aspirin, even in low doses, presents a similar concern.
Many medications impacting the liver’s ability to process drugs should be approached cautiously. These affect warfarin metabolism. Consult your doctor before using any new medication, particularly those metabolized by the liver.
| Medication Class | Examples | Interaction Type | Potential Risk |
|---|---|---|---|
| Antibiotics | Ciprofloxacin, Metronidazole | Increased Warfarin Effect | Increased bleeding |
| Antifungals | Ketoconazole, Itraconazole | Increased Warfarin Effect | Increased bleeding |
| NSAIDs | Ibuprofen, Naproxen | Increased Bleeding Risk | Increased bleeding, bruising |
| Aspirin | Aspirin | Increased Bleeding Risk | Increased bleeding, bruising |
| Amiodarone | Amiodarone | Variable Interaction | Requires close monitoring |
This table highlights some key interactions. This is not an exhaustive list. Always inform your doctor and pharmacist of all medications you are taking, including over-the-counter drugs and supplements. Regular blood tests are necessary to monitor your INR (International Normalized Ratio) while on warfarin.
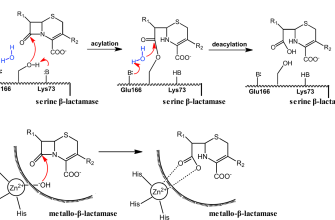
Understanding Warfarin’s Mechanism of Action
Warfarin inhibits vitamin K epoxide reductase, a crucial enzyme in the vitamin K cycle. This cycle is responsible for producing the active form of vitamin K, a necessary cofactor for the synthesis of several clotting factors: II, VII, IX, and X.
Impact on Clotting Factors
By blocking vitamin K epoxide reductase, warfarin prevents the activation of these clotting factors. This leads to a reduction in the production of functional clotting factors, thus decreasing blood clotting ability.
- Factor II (prothrombin): Converts into thrombin, essential for fibrin formation (blood clot).
- Factor VII: Initiates the extrinsic coagulation pathway.
- Factor IX: Part of the intrinsic coagulation pathway.
- Factor X (Stuart-Prower factor): Connects the intrinsic and extrinsic pathways, leading to thrombin formation.
Consequences of Reduced Clotting
The decreased production of these factors results in a prolonged prothrombin time (PT) and international normalized ratio (INR), which are used to monitor warfarin’s effectiveness. This therapeutic anticoagulation helps prevent blood clots in conditions like atrial fibrillation and deep vein thrombosis.
Factors Influencing Warfarin’s Effect
- Dietary Vitamin K intake: High vitamin K intake can counteract warfarin’s effects.
- Drug interactions: Many medications can either increase or decrease warfarin’s potency. Careful monitoring is vital.
- Genetic variations: Individual differences in metabolism affect warfarin’s response.
- Liver function: Liver health impacts the metabolism and clearance of warfarin.
Monitoring Warfarin Therapy
Regular blood tests measuring PT and INR are necessary to adjust warfarin dosage and maintain therapeutic anticoagulation while minimizing the risk of bleeding.
In Summary
Warfarin’s mechanism centers on inhibiting vitamin K recycling, subsequently reducing the production of crucial clotting factors and leading to controlled anticoagulation. This effect is influenced by various factors, emphasizing the need for close monitoring of therapy.
Nonsteroidal Anti-Inflammatory Drugs (NSAIDs) and Warfarin Interactions
Avoid combining NSAIDs like ibuprofen, naproxen, or celecoxib with warfarin. NSAIDs increase the risk of bleeding, and this risk is amplified when taken with warfarin, a blood thinner. This is because NSAIDs inhibit platelet aggregation, a process crucial for blood clot formation, similar to warfarin’s mechanism.
Increased Bleeding Risk
The combined effect can lead to serious, even life-threatening, bleeding complications such as gastrointestinal bleeding, hematuria (blood in urine), or intracranial hemorrhage. This heightened risk is particularly relevant for individuals already predisposed to bleeding issues or those taking higher warfarin doses. Close monitoring of your INR (International Normalized Ratio) is particularly important when using NSAIDs concurrently with warfarin. Regular blood tests are necessary to adjust warfarin dosage appropriately.
Alternatives to NSAIDs
If you require pain relief, discuss alternatives with your doctor. Acetaminophen (paracetamol) is generally a safer choice than NSAIDs when you are on warfarin, as it does not significantly affect platelet function or increase bleeding risk. Your physician can help determine the safest pain management strategy for your individual circumstances. Always inform your healthcare provider about all medications you are taking, including over-the-counter drugs.
Aspirin and Warfarin: A Risky Combination
Avoid combining aspirin and warfarin without your doctor’s explicit approval. This combination significantly increases your bleeding risk.
Aspirin, even in low doses, thins your blood, much like warfarin. Taking them together dramatically boosts this effect, potentially leading to dangerous internal or external bleeding, including gastrointestinal bleeding, bruising, and even stroke.
The risk is particularly high for individuals over 65 or those with pre-existing conditions like ulcers or kidney problems. Your doctor will consider your specific health profile to determine the safety of combining these medications.
If you’re prescribed warfarin and need pain relief, discuss alternatives with your physician. They may recommend acetaminophen (paracetamol) or other medications that don’t interact negatively with warfarin.
Regular blood tests to monitor your INR (International Normalized Ratio) are vital while on warfarin. These tests ensure your dosage is appropriate and reduces the risk of complications from medication interactions.
Open communication with your healthcare provider is crucial. Always inform them about all medications, supplements, and herbal remedies you’re taking to prevent potentially harmful interactions.
Antibiotics and the Risk of Increased Bleeding
Certain antibiotics can interact with warfarin, increasing your risk of bleeding. This interaction happens because some antibiotics affect how your liver metabolizes warfarin. A reduced metabolism leads to higher warfarin levels in your blood, which increases your risk of bleeding.
Antibiotics to Watch Out For
Some antibiotics known to potentially interact with warfarin include: macrolides (like erythromycin and clarithromycin), metronidazole, fluconazole, and sulfamethoxazole/trimethoprim (co-trimoxazole). This isn’t an exhaustive list, and other antibiotics may also cause interactions. Always inform your doctor or pharmacist about all medications you’re taking, including antibiotics, before starting a new prescription. They can assess potential interactions and adjust your warfarin dose accordingly.
Regular monitoring of your INR (International Normalized Ratio) is crucial while taking antibiotics alongside warfarin. Your doctor will likely schedule more frequent blood tests to ensure your INR remains within the therapeutic range. Promptly report any unusual bleeding or bruising to your healthcare provider.
Remember, the severity of the interaction depends on several factors, including the specific antibiotic, its dosage, and your individual response to warfarin. Open communication with your healthcare team is key to managing this potential risk.
Herbal Supplements and Warfarin: Potential for Dangerous Interactions
Avoid herbal supplements while taking warfarin. Many interact dangerously, increasing bleeding risk. This is because many herbs affect blood clotting, often in unpredictable ways.
Ginkgo biloba, for example, thins the blood, potentially causing excessive bleeding when combined with warfarin. Similarly, St. John’s wort can reduce warfarin’s effectiveness, leading to blood clots. Both supplements should be completely avoided.
Avoid also: Garlic, ginseng, ginger, chamomile, and dong quai. These herbs show potential for interactions, although research isn’t always conclusive on the extent of the risk. The safest approach is to avoid them.
Always consult your doctor or pharmacist before taking any herbal supplement or making dietary changes while on warfarin. They can help assess your individual risk and advise on safe alternatives. Your doctor will monitor your INR (international normalized ratio) regularly to ensure your warfarin dosage is appropriate and safe.
Open communication with your healthcare team is key. Inform them of all medications, supplements, and even over-the-counter drugs you’re taking. This enables them to make informed decisions about your treatment and minimize potential complications.
The Impact of Amiodarone on Warfarin’s Efficacy
Amiodarone significantly increases warfarin’s anticoagulant effect. This interaction stems from amiodarone’s inhibition of hepatic cytochrome P450 enzymes, specifically CYP2C9 and CYP3A4, which metabolize warfarin. Reduced warfarin metabolism leads to elevated warfarin levels in the blood.
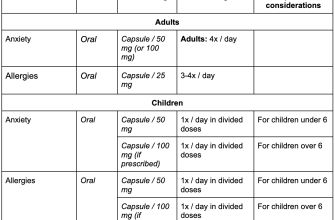
Expect a heightened risk of bleeding. This risk necessitates close monitoring of the International Normalized Ratio (INR). Frequent INR testing, often multiple times weekly, is necessary while patients are on both medications. Adjustments to warfarin dosage are frequently required to maintain the INR within the therapeutic range (typically 2.0-3.0 for most indications).
Dosage reductions of warfarin are typically needed. The magnitude of the reduction depends on individual patient factors, including age, liver function, and other concurrent medications. A physician’s expert guidance is crucial in managing this interaction. Ignoring this interaction can result in serious, even life-threatening, bleeding complications.
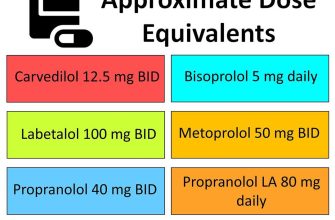
Consider alternative antiarrhythmics. If possible, explore alternative antiarrhythmic medications with less significant interactions with warfarin. Consult with a cardiologist and a hematologist to weigh the risks and benefits of each treatment option and to develop a comprehensive medication plan.
Monitor for signs of bleeding. Patients should be educated on the signs and symptoms of bleeding, including easy bruising, unusual nosebleeds, and black, tarry stools. Prompt medical attention is essential if bleeding occurs.
Monitoring Your Medications While on Warfarin
Maintain a detailed medication list. Include prescription drugs, over-the-counter medicines, supplements, and herbal remedies. Update this list whenever you begin or stop taking a medication.
Regularly check interactions: Many medications can affect warfarin’s effectiveness. Consult your pharmacist or doctor for medication reviews. They can identify potential interactions and adjust your warfarin dose accordingly.
- Common interacting medications include: NSAIDs (like ibuprofen), aspirin, antibiotics (especially certain types), antifungal medications, and some herbal supplements like St. John’s Wort.
- Never start or stop any medication without consulting your doctor or pharmacist. This is paramount for maintaining a stable INR level.
Undergo consistent INR monitoring. Your doctor will schedule regular blood tests to check your INR (international normalized ratio). This monitors how well warfarin thins your blood. Follow these scheduled appointments meticulously.
- Report any changes in your health promptly to your doctor, including unusual bleeding or bruising.
- Dietary consistency matters: Maintain a consistent diet regarding vitamin K intake, as it affects warfarin’s efficacy. Sudden changes can impact your INR.
- Inform all healthcare providers about your warfarin use, including dentists, before any procedures.
Carry a medication alert card or bracelet. This readily provides crucial information about your warfarin treatment to medical personnel in case of emergencies.
Actively participate in your treatment. Ask questions and express concerns. Your active engagement in your healthcare positively impacts your safety and well-being while on warfarin.
The Importance of Open Communication with Your Doctor
Share all medications you take, including over-the-counter drugs, supplements, and herbal remedies, with your doctor. This includes vitamins and even seemingly innocuous products like St. John’s Wort.
Regularly schedule check-up appointments to monitor your INR levels and discuss any changes in your health or medication regimen. This proactive approach helps prevent complications.
Report any new symptoms, side effects, or concerns immediately. Don’t wait for your next scheduled appointment. Prompt reporting can lead to quick adjustments to your treatment plan.
Maintain a detailed medication log, including dosages and dates. This will aid your physician in making accurate assessments and tracking potential interactions.
Ask questions! Don’t hesitate to clarify anything you don’t understand about your medication or treatment plan. Your doctor is there to help you.
Provide a complete medical history, including any allergies or previous adverse reactions to medications. This thoroughness is vital for safe and effective care.
Consider using a medication management app or tool to track your medications and appointments. This helps maintain organization and ensures you stay informed.
Actively participate in your care by being an informed patient. Your active role contributes significantly to positive health outcomes.
Consequences of Ignoring Contraindications: Bleeding Risks and Management
Ignoring warfarin contraindications significantly increases your bleeding risk. This risk manifests in various ways, from minor bruising and nosebleeds to life-threatening internal hemorrhages. The severity depends on the interacting medication and the individual’s health.
Recognizing Warning Signs
Watch for unusual bleeding or bruising. This includes bleeding gums, heavy menstrual bleeding, bloody or black stools, and unexplained nosebleeds. Seek immediate medical attention if you experience severe headache, dizziness, confusion, or vomiting blood. These can indicate internal bleeding requiring urgent intervention.
Managing Bleeding Complications
If bleeding occurs, immediately contact your doctor or go to the nearest emergency room. Treatment depends on the bleeding’s severity and location. It may include vitamin K administration to counteract warfarin’s anticoagulant effects, blood transfusions to replace lost blood, or surgical intervention to control internal bleeding. Prompt medical attention is crucial to minimize complications and potentially save your life.
Preventing Future Complications
Always inform your doctor and pharmacist of all medications, supplements, and herbal remedies you are taking. This allows them to identify potential interactions and adjust your warfarin dosage accordingly. Regular blood tests to monitor your INR (International Normalized Ratio) are also vital for maintaining a safe therapeutic range and minimizing bleeding risks. Active participation in your healthcare is essential for safe and effective warfarin management.