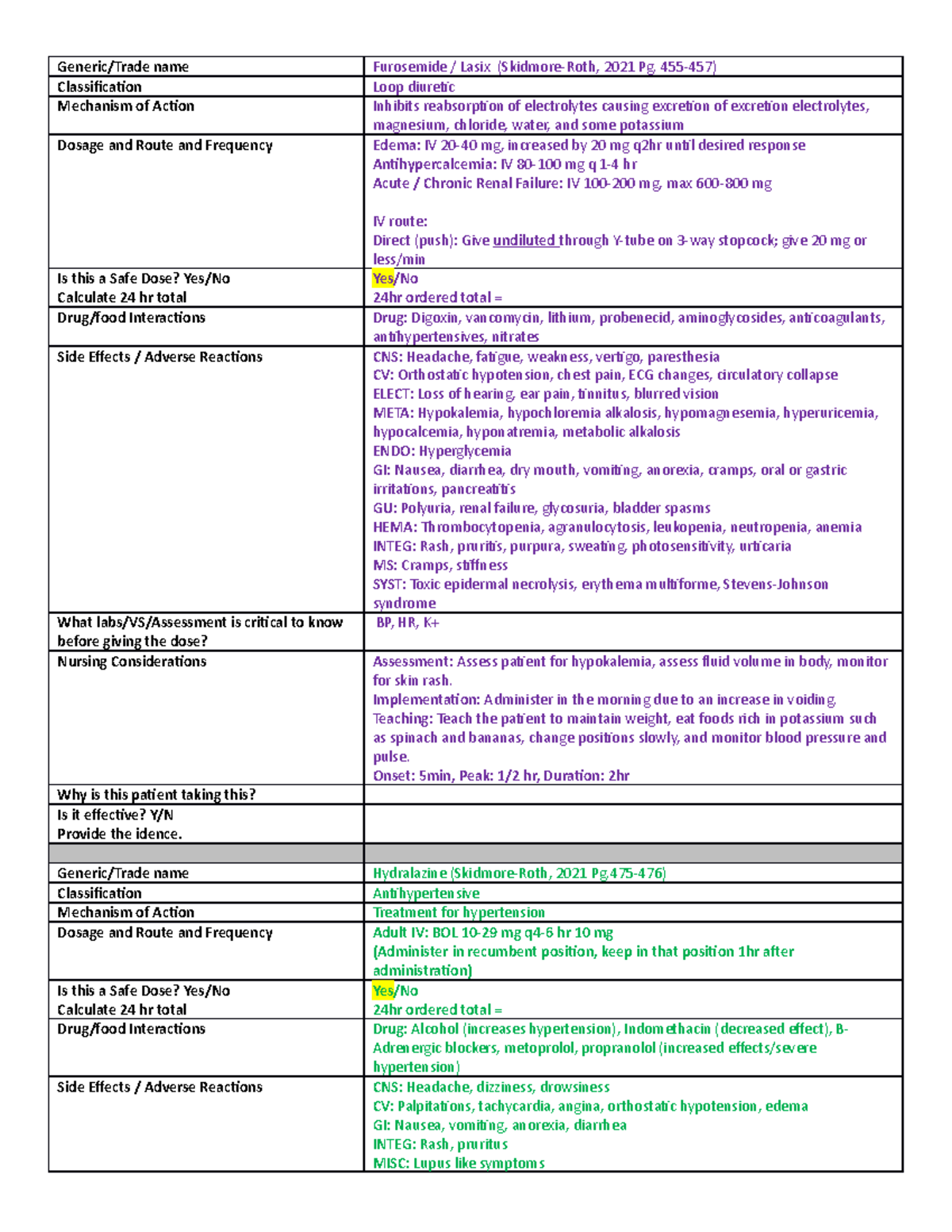
Administering Lasix over at least two minutes minimizes the risk of ototoxicity. Rapid infusion increases the likelihood of hearing damage, a serious adverse effect. This guideline protects patients and aligns with best practices.
Target a slower infusion rate of approximately 10-20 mg/minute, adjusting based on patient factors and available resources. Always check compatibility with other IV medications before mixing. Closely monitor the patient’s blood pressure and electrolyte levels during and after the infusion.
Documentation is key. Record the infusion rate, duration, any observed adverse effects, and the patient’s response. This detailed record provides a crucial safety net and facilitates proper medical care. Remember to consult official guidelines and package inserts for the most up-to-date information.
Note: This information serves as guidance and does not replace professional medical advice. Always consult with a qualified healthcare professional for specific instructions regarding Lasix administration.
- Lasix Pushed Over 2 Minutes to Avoid: A Detailed Analysis
- Understanding the Risks of Rapid Lasix Administration
- The Physiological Effects of Slow Versus Rapid Lasix Infusion
- Hypotension Risk
- Ototoxicity Concerns
- Clinical Scenarios Where Slow Lasix Administration is Crucial
- Practical Guidelines for Safe Lasix Administration
- Potential Legal and Ethical Implications of Rapid Lasix Infusion
- Legal Ramifications
- Ethical Considerations
- Ethical Violations
Lasix Pushed Over 2 Minutes to Avoid: A Detailed Analysis
Administering Lasix rapidly can cause profound hypotension and other adverse effects. Slow intravenous administration over at least two minutes is recommended to mitigate these risks.
Faster administration increases the risk of:
- Significant drops in blood pressure (hypotension)
- Dizziness and lightheadedness
- Transient deafness
- Arrhythmias
Optimal infusion rate: Individual patient needs vary, but a rate of 10-20 mg/minute is frequently used, subject to clinical judgement and continuous monitoring. Always consult the patient’s specific medical history and current condition.
Monitoring during administration is vital: Continuously track blood pressure, heart rate, and urine output. Closely observe the patient for any signs of discomfort or adverse reactions. Adjust the infusion rate as needed based on the patient’s response.
Pre-administration considerations: Assess renal function and hydration status before administering Lasix. Correct any electrolyte imbalances prior to drug administration. Consult medication interaction databases for any potential drug-drug interactions. Patients with pre-existing heart conditions require particularly careful monitoring.
Post-administration care: Observe the patient for at least 30 minutes post-infusion. Continue monitoring vital signs and patient response. Adequate hydration is crucial following Lasix administration.
Exceptions: In rare, emergency situations, faster administration may be necessary under strict medical supervision, but always prioritize patient safety and carefully consider potential risks and benefits.
Understanding the Risks of Rapid Lasix Administration
Administering Lasix rapidly can cause serious complications. Avoid pushing Lasix faster than 2 minutes.
Rapid infusion increases the risk of ototoxicity, a potentially irreversible hearing loss. This is due to the drug’s direct effect on the inner ear.
Sudden drops in blood pressure, known as hypotension, are another significant risk. This can lead to dizziness, fainting, and even kidney damage.
Dehydration is a common consequence of rapid Lasix administration. This is because Lasix promotes significant fluid loss. Electrolyte imbalances, particularly hypokalemia (low potassium), can result, leading to cardiac arrhythmias.
To mitigate these risks, always adhere to the recommended infusion rate. Monitor the patient closely for any signs of hypotension, ototoxicity, or electrolyte imbalances. Regularly check blood pressure and potassium levels. Immediate intervention is necessary if complications arise.
Always consult the current drug monograph for complete details on safe administration protocols. Patient-specific factors influence the optimal infusion rate.
The Physiological Effects of Slow Versus Rapid Lasix Infusion
Administering Lasix slowly, over at least two minutes, significantly reduces the risk of hypotension and ototoxicity compared to rapid bolus injection. This slower infusion allows for a more gradual diuresis, preventing a sudden drop in blood volume and pressure. Rapid infusion, conversely, can overwhelm the circulatory system, leading to a precipitous decrease in blood pressure, potentially causing dizziness, syncope, and even cardiac events.
Hypotension Risk
Studies show a direct correlation between the rate of Lasix administration and the incidence of hypotension. A slower infusion rate allows the body to compensate for fluid loss more effectively, minimizing the severity of hypotensive episodes. Specific infusion rates should be tailored to the individual patient’s condition and response, but a rate exceeding 40 mg/minute is generally discouraged.
Ototoxicity Concerns
Rapid Lasix infusion can also increase the risk of ototoxicity, particularly in patients with pre-existing renal impairment. Slow administration minimizes the peak plasma concentration of the drug, thereby reducing the potential for damaging effects on the inner ear. Monitoring serum creatinine and electrolytes helps guide safe administration.
Clinical Scenarios Where Slow Lasix Administration is Crucial
Administering Lasix slowly, over at least two minutes, is vital in several situations to mitigate potential adverse effects. This approach significantly reduces the risk of potentially life-threatening complications.
Rapid Lasix infusion can cause profound hypotension, particularly in patients with pre-existing conditions such as hypovolemia, heart failure, or renal impairment. A slow infusion allows for better hemodynamic monitoring and adjustment, preventing sudden drops in blood pressure.
Ototoxicity, characterized by tinnitus and hearing loss, is another significant concern with rapid Lasix administration. A slower infusion rate reduces the concentration of Lasix reaching the inner ear, diminishing this risk.
For patients with electrolyte imbalances, particularly hypokalemia, slow administration is crucial. Rapid Lasix infusion can exacerbate existing electrolyte abnormalities, leading to potentially serious cardiac arrhythmias. A slower infusion allows for better monitoring and correction of electrolyte imbalances.
| Clinical Situation | Reason for Slow Administration |
|---|---|
| Hypovolemia | Reduces risk of severe hypotension |
| Heart Failure (severe) | Minimizes abrupt decreases in blood pressure |
| Renal Impairment | Allows for better fluid balance management |
| Pre-existing electrolyte imbalances (e.g., hypokalemia) | Prevents further electrolyte disruption and arrhythmias |
| Older adults | Reduced risk of adverse effects due to age-related physiological changes |
Always monitor vital signs closely during and after Lasix administration, regardless of infusion rate. Adjustments to the rate and dose might be necessary based on patient response. Consult prescribing information for further details and always prioritize patient safety.
Practical Guidelines for Safe Lasix Administration
Always verify the patient’s identity using two identifiers before administering Lasix.
Check for allergies and contraindications. Review the patient’s medical history, including renal function and electrolyte levels.
Calculate the correct dose based on patient weight and medical condition. Double-check calculations with another nurse.
Administer Lasix intravenously slowly, over at least two minutes, to reduce the risk of hypotension. Rapid administration can cause serious complications.
Monitor blood pressure and heart rate closely during and after administration. Observe for signs of hypotension, such as dizziness or lightheadedness.
Monitor fluid balance and electrolyte levels, especially potassium, regularly. Lasix can cause hypokalemia.
Educate the patient about potential side effects, such as dehydration, dizziness, and muscle weakness. Encourage them to report any adverse reactions immediately.
Document the administration accurately, including dose, route, time, and patient response. Note any significant observations.
Be aware of potential drug interactions. Consult drug references for relevant information.
If intravenous administration is not feasible, follow the same careful procedures for oral administration. Ensure the patient can swallow the medication safely.
In case of accidental overdose, follow established emergency protocols immediately. Contact medical control for guidance.
Potential Legal and Ethical Implications of Rapid Lasix Infusion
Administering Lasix rapidly carries significant legal and ethical risks. Failure to adhere to recommended infusion rates can lead to serious adverse events, potentially resulting in malpractice lawsuits.
Legal Ramifications
- Negligence: Rapid infusion increasing the risk of hypovolemia, hypotension, or electrolyte imbalances can constitute negligence if it deviates from established standards of care. Documentation meticulously outlining the rationale for any deviation is crucial for legal defense.
- Battery: Administering medication against a patient’s informed consent, even if indirectly via exceeding recommended infusion rates and causing harm, can be considered battery. Explicit consent for the specific administration method must be documented.
- Liability: Hospitals and healthcare providers can face substantial financial liability from resulting injuries, including compensation for medical expenses, lost wages, and pain and suffering. Thorough incident reporting and internal investigation are paramount.
Ethical Considerations
Beyond legal repercussions, rapid Lasix infusion raises ethical concerns:
Ethical Violations
- Beneficence: The principle of acting in the patient’s best interest is violated by increasing risks through rapid administration. A slower, safer infusion aligns with this principle.
- Non-maleficence: The obligation to “do no harm” is compromised by unnecessarily increasing the risk of complications. Careful attention to infusion rates directly addresses this ethical duty.
- Autonomy: While informed consent might be obtained, failing to fully disclose the risks associated with rapid administration infringes on the patient’s right to make informed choices about their treatment.
Strict adherence to established guidelines and careful documentation are essential to mitigate these risks. Thoroughly review protocols, prioritize patient safety, and maintain meticulous records. Consulting with colleagues when uncertain about appropriate administration is encouraged.