Express Scripts’ coverage of Accutane (isotretinoin) varies significantly. Your specific plan determines whether you’ll receive coverage, and the extent of that coverage. Check your formulary–that’s your plan’s official drug list–or contact Express Scripts directly to confirm.
Prior authorization is almost always required. This means your doctor needs to submit additional information justifying the need for Accutane before Express Scripts approves the prescription. Be proactive; discuss this with your dermatologist well in advance of needing the medication. They can guide you through the process and improve your chances of approval.
Cost-sharing–your out-of-pocket expenses–will depend on your plan’s tier system. Accutane is often a higher-cost medication, placing it in a tier requiring substantial co-pays or coinsurance. Your plan documents will outline your financial responsibility. Explore manufacturer coupons or patient assistance programs if cost is a barrier; these resources could significantly reduce your expenses.
Remember: This information is for guidance only; always consult your insurance provider for precise details concerning your coverage. They are the definitive source for your specific plan’s benefits.
- Does Express Scripts Cover Accutane?
- Express Scripts Formulary and Accutane Coverage
- Prior Authorization Requirements for Accutane
- Gathering Necessary Information
- Timing and the Approval Process
- Appealing a Denied Request
- Factors Affecting Accutane Coverage by Express Scripts
- Cost of Accutane with and without Express Scripts Coverage
- Alternatives to Accutane and Their Coverage by Express Scripts
- Appealing a Denied Accutane Claim with Express Scripts
Does Express Scripts Cover Accutane?
Coverage for Accutane (isotretinoin) through Express Scripts depends entirely on your specific insurance plan. Accutane is a high-cost medication with stringent requirements due to its potential side effects. Therefore, prior authorization is almost always necessary.
Check your Express Scripts formulary online or contact your plan administrator directly. Your formulary details your plan’s covered medications and any restrictions. The administrator can clarify Accutane’s coverage status, outlining any steps required for pre-authorization.
Pre-authorization typically involves providing medical records demonstrating the need for Accutane. This might include dermatologist reports outlining your acne severity and response to other treatments. Be prepared to share this information promptly to expedite the process.
If your plan doesn’t cover Accutane, consider exploring patient assistance programs offered by the manufacturer or other charitable organizations. These programs often help reduce medication costs for eligible patients.
Remember, your specific situation will influence whether your plan covers Accutane. Actively communicating with your insurance provider is key to understanding your coverage options and ensuring access to the medication.
Express Scripts Formulary and Accutane Coverage
Accutane coverage through Express Scripts depends entirely on your specific plan. There’s no single answer.
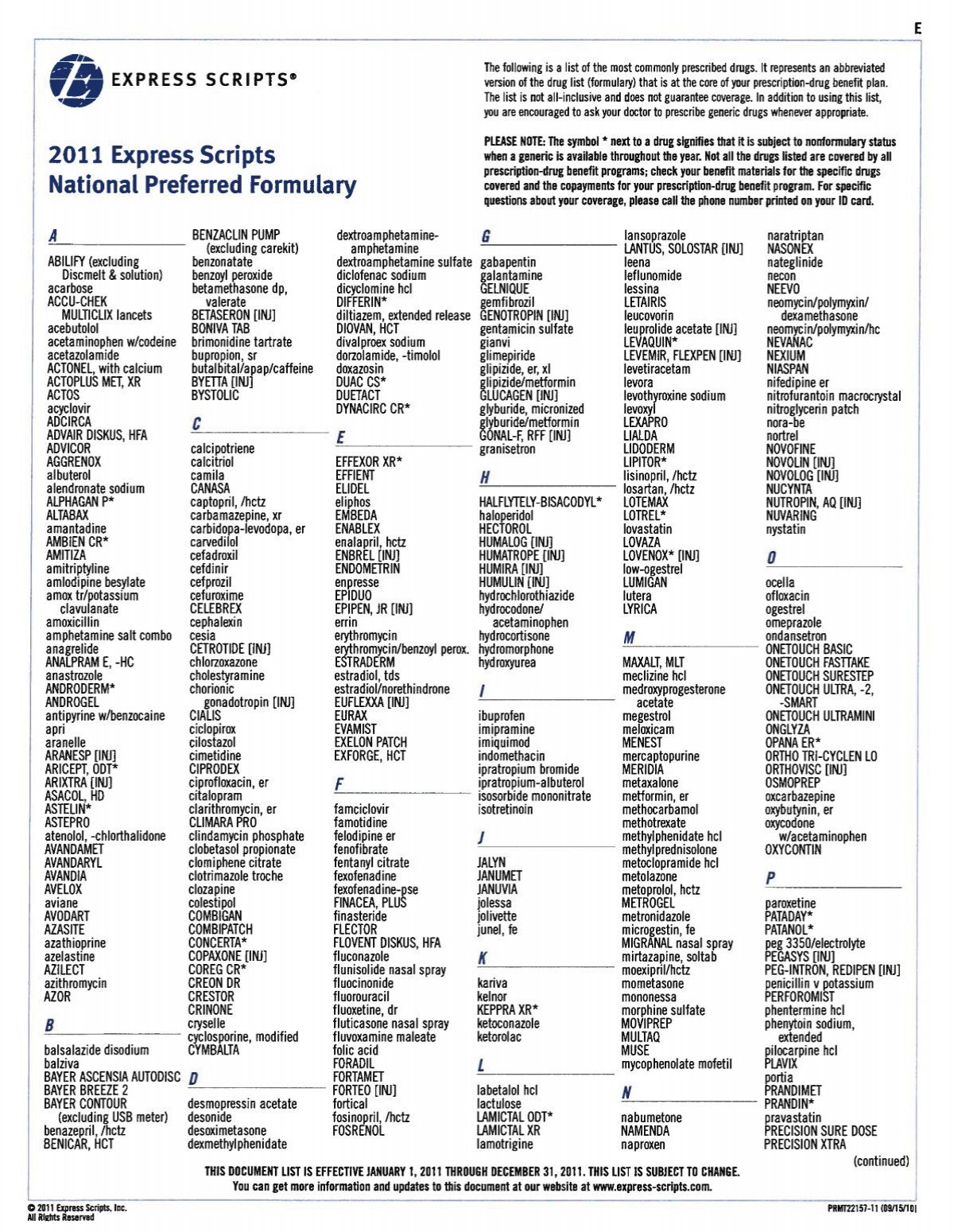
Check your plan’s formulary. This document lists covered medications. Access it online through your Express Scripts member portal or contact your plan administrator.
- Locate the formulary: Your plan’s website provides a link. You’ll likely need your member ID and password.
- Search for “isotretinoin”: This is the generic name for Accutane.
- Review coverage details: Note any prior authorization requirements, step therapy protocols, or cost-sharing information (copay, deductible, etc.).
If Accutane isn’t listed or requires prior authorization, contact your doctor. They can submit a request on your behalf, explaining the medical necessity. This might involve providing supporting documentation like medical records.
Consider these factors influencing coverage:
- Your insurance plan type: Employer-sponsored plans, Medicare Part D plans, or individual plans all have varying formularies and coverage criteria.
- Your specific health needs: The severity of your acne and response to other treatments might affect the approval process.
- Generic vs. brand-name: Express Scripts generally prefers generic medications, so isotretinoin might be covered more favorably than Accutane.
Prepare for potential challenges. Coverage decisions may vary. Be proactive in communicating with your doctor and Express Scripts.
Prior Authorization Requirements for Accutane
Contact Express Scripts directly to confirm current requirements. Their specific guidelines change, so always obtain the most up-to-date information.
Gathering Necessary Information
You’ll need your doctor to submit detailed information. This typically includes a completed prior authorization form, patient demographics, a detailed treatment plan outlining the rationale for Accutane, and results of pregnancy tests (for female patients). Confirm all required documentation with your doctor and Express Scripts.
Timing and the Approval Process
Expect a delay. The review process usually takes several days to a couple of weeks. Express Scripts may request additional information, potentially extending the timeframe. Follow up with your doctor and pharmacy to track the status of your request.
Appealing a Denied Request
If your prior authorization is denied, understand Express Scripts’ reasons. Your doctor can then submit a detailed appeal including supporting medical evidence. This process may involve additional documentation and further review.
Factors Affecting Accutane Coverage by Express Scripts
Express Scripts’ coverage of Accutane (isotretinoin) hinges on several key factors. Understanding these helps you prepare for the prescription process.
First, prior authorization is almost always required. This involves your dermatologist submitting detailed information to Express Scripts justifying the need for Accutane. Failure to provide complete documentation often results in denial. Ensure your doctor provides all requested medical records, including severity assessments and prior treatment attempts.
Second, your insurance plan dictates specifics. Express Scripts manages pharmacy benefits for many insurance providers, but each plan differs. Your copay, deductible, and even drug coverage levels vary widely depending on your plan’s formulary and tier placement of Accutane. Check your Summary of Benefits and Coverage (SBC) for details.
Third, patient adherence to iPledge, the mandatory risk management program for Accutane, is crucial for coverage. You must enroll and follow all program guidelines, including regular pregnancy tests and monthly check-ins with your dermatologist. Non-compliance directly impacts coverage approval.
Finally, alternative treatment failures are significant. Express Scripts often requires documentation showing that other acne treatments have been tried unsuccessfully before Accutane is considered. Keep detailed records of previous treatments, including their duration and results.
| Factor | Impact on Coverage | Recommendation |
|---|---|---|
| Prior Authorization | Often required; denial without complete documentation. | Ensure your doctor provides comprehensive medical records. |
| Insurance Plan | Determines copay, deductible, and coverage levels. | Review your SBC for specifics on Accutane coverage. |
| iPledge Adherence | Non-compliance leads to coverage denial. | Strictly follow all iPledge guidelines. |
| Alternative Treatment History | Documentation of failed treatments is often needed. | Maintain thorough records of previous acne treatments. |
Proactive communication with your dermatologist and insurance provider streamlines the process and enhances the likelihood of coverage approval.
Cost of Accutane with and without Express Scripts Coverage
Accutane’s price varies significantly. Expect to pay between $800 and $2000 per month without Express Scripts coverage. This is a broad range due to factors like dosage and pharmacy.
With Express Scripts coverage, your out-of-pocket expenses depend heavily on your specific plan. A copay could range from $0 to several hundred dollars per month. Your plan’s deductible and coinsurance significantly impact your final cost.
To determine your precise cost: Check your Express Scripts formulary for Accutane (isotretinoin). Contact Express Scripts directly or your insurance provider for detailed cost information, including any applicable copays, deductibles, and prior authorizations. They can provide a personalized estimate.
Consider these factors: Your specific Express Scripts plan, your deductible status, and the quantity of Accutane prescribed will all influence your expenses. Pharmacy pricing also plays a role; consider using a preferred pharmacy.
Saving money: Explore patient assistance programs offered by Roche, the manufacturer of Accutane. These programs may offer financial assistance to reduce your out-of-pocket costs. Always carefully review program eligibility requirements.
Remember, these are estimates. Accurate cost calculation requires direct communication with your insurance provider and pharmacy.
Alternatives to Accutane and Their Coverage by Express Scripts
Express Scripts’ coverage for Accutane alternatives varies greatly depending on your specific plan and location. Always check your formulary for the most up-to-date information. However, generally, they cover some oral and topical retinoids. Oral retinoids like isotretinoin (although brand name Accutane is rarely covered) might require prior authorization. You’ll find that topical retinoids, such as tretinoin, adapalene, and tazarotene, are usually covered with a lower copay.
For other treatments, coverage differs significantly. Antibiotics, such as doxycycline or minocycline, commonly prescribed for acne, are generally covered, but again, prior authorization may be needed. Hormonal therapies, like birth control pills used for acne management, have varying coverage levels. This necessitates directly contacting Express Scripts or your physician for accurate details.
Before switching treatments, consult with your dermatologist. They can explain the advantages and disadvantages of each alternative and help determine which treatment best suits your needs and insurance coverage. Your doctor can also help navigate the prior authorization process if required.
Remember that prices and coverage can change, so confirming directly with Express Scripts before starting any new medication is highly recommended.
Appealing a Denied Accutane Claim with Express Scripts
Begin by carefully reviewing your denial letter. Identify the specific reason for the denial. This is crucial for crafting your appeal.
Gather all necessary supporting documentation. This includes:
- Your doctor’s prescription
- Detailed medical records demonstrating severe acne and treatment failure with other medications
- Photos of your acne (before and during treatment attempts)
- Any prior authorizations or communications with Express Scripts
Contact your dermatologist. They can provide additional information and potentially write a stronger appeal letter emphasizing the severity of your acne and the need for Accutane. Their support is invaluable.
Express Scripts provides a formal appeals process. Follow their instructions meticulously. Clearly state the reason for your appeal, referencing specific points in your denial letter and providing the supporting documentation. Be polite but firm.
If your initial appeal is denied, explore the next steps within Express Scripts’ appeals process. Their website should outline further options. Consider consulting with a patient advocate who specializes in medication appeals if needed.
Maintain detailed records of all communication with Express Scripts, including dates, times, and the names of anyone you speak with. This documentation will be helpful in subsequent steps.
Remember, persistence often pays off. Don’t hesitate to thoroughly follow the appeals process. Your dermatologists’ continued support is key.