Doctors discontinue tetracycline prescriptions primarily due to the emergence of resistant bacteria and the drug’s potential for adverse effects. Antibiotic resistance is a serious global health threat, and tetracycline’s widespread use has contributed to the development of strains that no longer respond to its action. This necessitates exploring alternative treatment options.
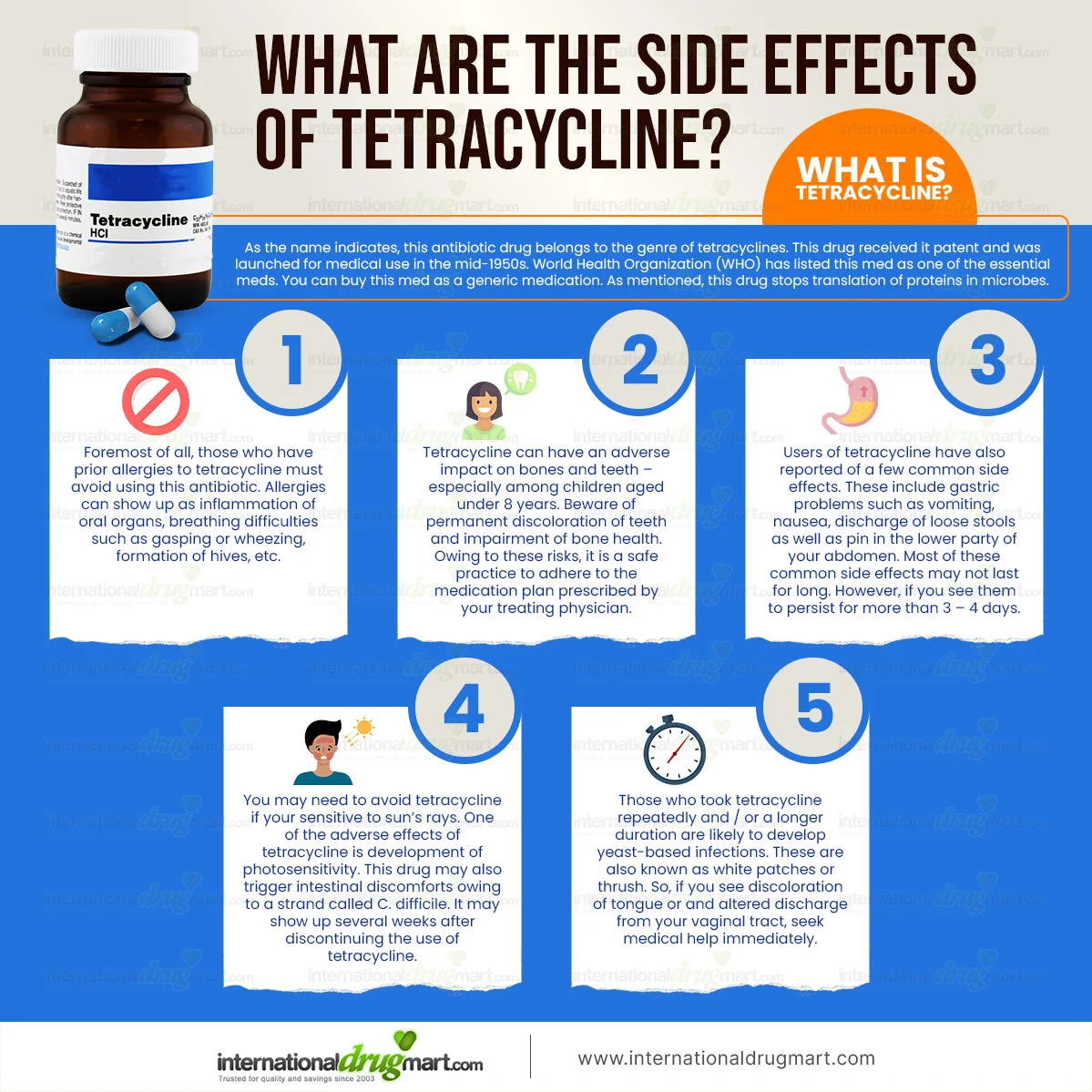
Specifically, tetracycline’s side effects, including gastrointestinal issues like nausea and diarrhea, tooth discoloration in children, and photosensitivity, often outweigh the benefits in certain cases. These factors, coupled with the growing resistance problem, lead physicians to carefully consider other antibiotics with a potentially better safety profile and efficacy against the specific infection. Careful assessment of the patient’s medical history and the bacterial infection is crucial before prescribing any antibiotic.
Consider this: If a less toxic antibiotic with comparable effectiveness is available to treat the infection, it often becomes the preferred choice. Always consult your physician or other qualified healthcare provider if you have concerns about your antibiotic prescription or experience any adverse effects. They can provide personalized advice and determine the most suitable treatment plan for your unique circumstances. They will take into account the severity of your infection, the type of bacteria involved and your overall health.
- Why is Tetracycline Discontinued?
- Development of Resistance in Bacteria
- Ineffective Against Certain Bacterial Infections
- Toxicity and Side Effects
- Liver Toxicity
- Dental Discoloration
- Photosensitivity
- Other Side Effects
- Important Note
- Drug Interactions
- Interactions with Specific Medications
- Availability of Newer, Safer Antibiotics
- Concerns Regarding Tooth Staining
- Potential for Liver Damage
- Impact on Bone Growth in Children
- Tooth Discoloration
- Bone Growth Inhibition
- Dosage and Timing
- Alternatives
- Monitoring
- Alternative Treatment Options
Why is Tetracycline Discontinued?
Doctors discontinue tetracycline prescriptions primarily due to the drug’s potential for causing permanent tooth discoloration in developing children and pregnant women. This discoloration is especially problematic in young children, affecting the developing enamel.
Another significant reason for discontinuation is the emergence of resistant bacteria. Tetracycline’s effectiveness has diminished over time as bacteria adapt. This means it may be less reliable in treating infections compared to newer antibiotics.
Furthermore, tetracycline can interact negatively with other medications, potentially leading to harmful consequences. Careful consideration of other prescriptions is therefore necessary before prescribing it. For example, it may decrease the efficacy of oral contraceptives.
Finally, some patients experience side effects including nausea, vomiting, and diarrhea. While not always severe, these gastrointestinal issues can significantly impact quality of life, leading doctors to consider alternatives.
In short, a combination of staining potential, bacterial resistance, drug interactions, and side effects often results in the discontinuation of tetracycline treatment in favor of safer and more effective antibiotics.
Development of Resistance in Bacteria
Tetracycline’s decline stems largely from bacterial resistance. Bacteria adapt through several mechanisms, making antibiotics less effective.
- Enzyme Production: Bacteria produce enzymes that break down tetracycline, rendering it inert.
- Efflux Pumps: These pumps actively expel tetracycline from the bacterial cell before it can act.
- Target Modification: Bacteria alter the structure of the ribosomal subunits that tetracycline targets, reducing its binding affinity.
- Reduced Permeability: Changes in the bacterial cell wall decrease tetracycline’s ability to enter the cell.
Resistance genes often reside on plasmids, small, transferable DNA loops. This allows rapid spread of resistance among bacterial populations, accelerating the decline of antibiotic efficacy.
- Overuse of antibiotics promotes selective pressure, favoring resistant strains and accelerating resistance development.
- Incomplete antibiotic courses allow resistant bacteria to survive and multiply.
- Agricultural use of tetracycline contributes significantly to the spread of resistance genes in the environment.
Careful antibiotic stewardship, including appropriate prescribing practices and infection control measures, is vital to slow the development and spread of bacterial resistance. Regular monitoring of resistance patterns guides future antibiotic use strategies.
Ineffective Against Certain Bacterial Infections
Tetracycline’s usefulness is limited by its inability to combat certain bacterial infections. Resistance mechanisms developed by bacteria, such as enzymatic inactivation or ribosomal protection, render tetracycline ineffective. Pseudomonas aeruginosa, a common cause of hospital-acquired infections, often displays resistance. Similarly, many strains of Enterococcus and Staphylococcus aureus, including methicillin-resistant S. aureus (MRSA), exhibit tetracycline resistance.
Specifically, Mycoplasma pneumoniae, a frequent cause of atypical pneumonia, shows reduced susceptibility. This limitation necessitates alternative antibiotic choices for these infections. Doctors now routinely perform susceptibility testing to guide treatment decisions, confirming whether tetracycline will be a viable option before prescribing it.
Always consult a medical professional for diagnosis and treatment. Self-treating bacterial infections is dangerous and can lead to complications. A physician will guide you toward appropriate antibiotics based on the specific bacteria identified and its susceptibility profile, ensuring the best chance of successful treatment. Failure to use the correct antibiotic can prolong illness and contribute to the spread of antibiotic-resistant bacteria.
The rise of antibiotic resistance necessitates careful antibiotic stewardship. Understanding tetracycline’s limitations is key to responsible antibiotic use and preventing further development of resistant strains.
Toxicity and Side Effects
Tetracycline’s discontinuation often stems from its potential for adverse reactions. Gastrointestinal distress, including nausea, vomiting, and diarrhea, is common. These issues are usually mild and resolve with continued treatment, but severe cases can require discontinuation.
Liver Toxicity
Rarely, tetracycline can cause liver damage. This risk is elevated in patients with pre-existing liver conditions or those taking other hepatotoxic medications. Monitor liver function tests if prescribed tetracycline, especially during prolonged therapy. Report any signs of liver problems, like jaundice (yellowing of skin and eyes) or dark urine, immediately.
Dental Discoloration
Tetracycline can permanently stain developing teeth a yellow-gray or brown color. This risk is highest in children under eight and pregnant women during the third trimester. Therefore, its use in these populations is generally avoided. If tooth staining occurs, professional dental cleaning might help, but complete removal is rarely possible.
Photosensitivity
Tetracycline increases skin sensitivity to sunlight. Sunburns are more likely, even with minimal sun exposure. Patients should use sunscreen with a high SPF, wear protective clothing, and limit sun exposure while taking tetracycline. Severe sunburns require immediate medical attention.
Other Side Effects
Less frequent side effects include yeast infections, kidney problems, and allergic reactions (ranging from mild rashes to life-threatening anaphylaxis). Any new or worsening symptoms should be reported to your doctor promptly. They can assess the severity of the reaction and determine the best course of action.
Important Note
This information is for educational purposes only and does not constitute medical advice. Always consult your doctor or pharmacist before starting or stopping any medication, including tetracycline. They can assess your individual risk factors and determine if tetracycline is the appropriate treatment option for you.
Drug Interactions
Tetracycline’s absorption can be significantly reduced by taking it with calcium, iron, magnesium, or aluminum-containing products. This includes antacids, milk, and some multivitamins. Space these medications at least two hours apart from your tetracycline dose to maximize absorption.
Interactions with Specific Medications
Certain antibiotics, like penicillin, can decrease tetracycline’s effectiveness. Conversely, tetracycline can reduce the effectiveness of oral contraceptives. Discuss these potential interactions with your doctor if you’re taking either of these types of medication. Methotrexate interactions are also possible; careful monitoring is required if you are on both.
Warfarin’s effects can be enhanced when combined with tetracycline, leading to increased bleeding risk. Close monitoring of your INR is critical if you’re on both medications. Finally, be aware that tetracycline can interact with some blood pressure medications, potentially affecting their efficiency. Always inform your doctor about all medications you’re taking, including over-the-counter drugs and supplements.
Availability of Newer, Safer Antibiotics
Tetracycline’s decline stems partly from the development of newer antibiotics with improved safety profiles and broader efficacy. Many modern alternatives offer better tolerance, reduced side effects, and targeted action against specific bacteria.
- Fluoroquinolones (e.g., Ciprofloxacin, Levofloxacin): These treat a wider range of bacterial infections than tetracycline, including some resistant strains. However, they carry potential risks of tendonitis and peripheral neuropathy, requiring careful consideration of benefits versus risks.
- Macrolides (e.g., Erythromycin, Azithromycin): These are generally well-tolerated and effective against various gram-positive bacteria. They are often preferred for patients with tetracycline allergies or intolerances. However, resistance is increasing.
- Cephalosporins (e.g., Ceftriaxone, Cefepime): This broad class covers numerous generations, each with expanding antimicrobial activity. They offer alternatives for severe infections where tetracycline might be inadequate. Like other antibiotics, careful monitoring for potential allergic reactions is crucial.
- Aminoglycosides (e.g., Gentamicin, Tobramycin): These are powerful antibiotics, particularly effective against gram-negative bacteria. However, they are generally reserved for serious infections due to potential kidney and hearing damage.
Selecting the right antibiotic always requires a doctor’s assessment. Factors like the specific bacteria causing the infection, the patient’s medical history, and potential drug interactions all play a role. Always consult a healthcare professional for diagnosis and treatment.
- Discuss your medical history and allergies with your physician.
- Provide a complete description of your symptoms.
- Follow your doctor’s prescribed dosage and duration of treatment meticulously.
- Never self-medicate or stop antibiotic use prematurely.
While newer antibiotics offer advantages, responsible use remains vital to combat antimicrobial resistance. This includes completing prescribed courses, avoiding unnecessary antibiotic use, and promoting infection prevention practices. This collaborative approach is key to preserving the effectiveness of these vital medications.
Concerns Regarding Tooth Staining
Tetracycline’s ability to stain developing teeth is a significant concern. This discoloration ranges from a mild yellow to a more pronounced brown or gray hue, affecting both primary and permanent teeth.
The staining occurs because tetracycline binds to the calcium in tooth enamel during tooth development. This means that children under eight years old and pregnant or breastfeeding women are particularly vulnerable because their teeth are still forming. The risk increases with the duration and dosage of tetracycline use.
Minimizing staining requires careful consideration. Your doctor will likely prescribe alternative antibiotics if possible, especially for children and pregnant women. If tetracycline is necessary, the shortest effective course is crucial. Good oral hygiene, including regular brushing and flossing, can help, but it won’t prevent staining entirely.
Professional cleaning and possibly bleaching may be options after tooth development is complete. However, these treatments don’t always completely remove the stains. The severity of the staining varies depending on multiple factors, including the dosage, duration of treatment, and the individual’s genetic predisposition.
Open communication with your doctor is key. Discuss potential risks and alternatives before starting any tetracycline treatment. This proactive approach helps you make informed decisions regarding your oral health.
Potential for Liver Damage
Tetracycline’s potential to harm the liver is a serious concern. While rare, liver damage can range from mild to severe. Cases of jaundice, elevated liver enzymes, and even acute liver failure have been reported. This risk is amplified in patients with pre-existing liver conditions or those taking multiple medications concurrently.
Regular monitoring of liver function is vital. Blood tests measuring liver enzyme levels (ALT and AST) should be conducted before starting tetracycline therapy and periodically throughout treatment, especially in high-risk individuals. Immediate discontinuation of tetracycline is necessary if abnormal liver function tests arise or symptoms like jaundice (yellowing of the skin or eyes), dark urine, or unusual fatigue develop. Early detection significantly improves the chances of a favorable outcome.
| Symptom | Action |
|---|---|
| Jaundice (yellowing of skin/eyes) | Stop taking tetracycline; seek immediate medical attention. |
| Dark urine | Stop taking tetracycline; contact your doctor. |
| Unusual fatigue | Stop taking tetracycline; consult your physician. |
| Abdominal pain | Stop taking tetracycline; seek medical advice. |
Specific risk factors like age, underlying health conditions, and concurrent medication use should be carefully considered before prescribing tetracycline. Consult a healthcare professional to assess your individual risk and weigh the benefits against the potential liver-related side effects.
Impact on Bone Growth in Children
Tetracycline’s impact on bone growth in children is a serious concern. It can cause discoloration of teeth, especially in children under 8 years old, whose teeth are still developing. This discoloration ranges from mild yellowing to a more pronounced brownish-gray hue, potentially impacting a child’s self-esteem. The staining is permanent.
Tooth Discoloration
Studies show a direct correlation between tetracycline use during tooth development and subsequent discoloration. The severity depends on factors like the dosage, duration of use, and the child’s age. Early exposure carries the highest risk of severe staining. The discoloration isn’t limited to the visible portion of the teeth; it can affect the underlying dentin, making it irreversible. There’s no reliable way to reverse tetracycline-stained teeth.
Bone Growth Inhibition
Beyond teeth, tetracycline can also affect bone growth, though this is less common than tooth staining. It can lead to hypoplasia, a condition marked by stunted bone growth, resulting in bones that are smaller and weaker than normal. While less frequent than tooth discoloration, this effect can have long-term consequences for a child’s skeletal development. Therefore, careful consideration of the risks is necessary.
Dosage and Timing
| Factor | Effect on Bone Growth |
|---|---|
| High Dosage | Increased risk of bone growth abnormalities |
| Long Treatment Duration | Increased risk of bone growth abnormalities |
| Age at Treatment | Younger children face higher risk due to ongoing bone development |
Alternatives
Doctors now prioritize safer alternatives whenever possible, minimizing tetracycline use in children. This cautious approach aims to protect developing bones and teeth. Always discuss treatment options thoroughly with your child’s pediatrician before starting any antibiotic course.
Monitoring
Regular check-ups are crucial for children treated with tetracycline. Monitoring for any signs of bone or teeth abnormalities is essential to manage potential complications effectively. Early detection allows for timely intervention and management of any arising issues.
Alternative Treatment Options
Your doctor will determine the best alternative depending on your specific infection and medical history. However, several classes of antibiotics often replace tetracycline.
- Doxycycline: This is a tetracycline-class antibiotic, but it often has better tolerability and longer half-life. It treats many of the same infections as tetracycline.
- Minocycline: Another tetracycline, sometimes preferred for its effectiveness against certain bacteria.
If tetracycline was prescribed for acne, other options include:
- Topical retinoids: These are applied directly to the skin and help reduce inflammation and prevent breakouts. Examples include tretinoin and adapalene.
- Benzoyl peroxide: A topical medication that kills acne-causing bacteria.
- Azelaic acid: Another topical treatment that reduces inflammation and bacteria.
- Oral antibiotics: Besides tetracyclines, your dermatologist might prescribe erythromycin or clindamycin for moderate to severe acne.
- Isotretinoin (Accutane): A powerful oral medication used for severe, treatment-resistant acne. It has potential side effects, requiring close monitoring by a dermatologist.
For other infections previously treated with tetracycline, alternatives might include:
- Amoxicillin: A penicillin-class antibiotic, suitable for a range of bacterial infections.
- Cephalosporins: This antibiotic class includes various drugs, like cefuroxime and ceftriaxone, effective against a wide array of bacteria.
- Macrolides (e.g., azithromycin, erythromycin): These are useful for infections where penicillin allergies exist.
Remember, always discuss treatment options with your physician. They can assess your individual needs and choose the most suitable and safe alternative to tetracycline.